Association between reproductive history, healthy lifestyle and cardiovascular disease in rural elder women with hypertension
-
摘要:
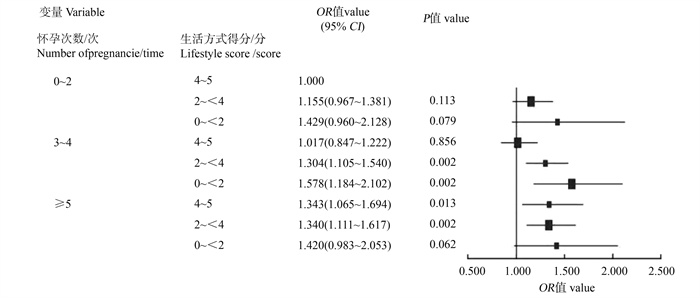
目的 探究≥65岁农村地区女性高血压患者生育史、生活方式与患心血管病(cardiovascular disease, CVD)风险的关系,并进一步探讨二者的联合作用。 方法 采用整群抽样方法,于2023年7―8月对河南省某县老年女性高血压患者进行问卷调查和体格检查。生育史包括怀孕次数、活产婴儿数和流产史,生活方式包括睡眠、饮食、体力活动、被动吸烟和BMI。采用logistic回归分析生育史、生活方式以及二者的联合作用对农村地区老年女性患CVD风险的影响。 结果 纳入分析的研究对象共9 837人,CVD患者3 980人。Logistic回归分析结果显示,怀孕≥5次、有流产史者患CVD的风险分别增加19.8%(OR=1.198, 95% CI: 1.057~1.359)、26.1%(OR=1.261, 95% CI: 1.151~1.381),生活方式得分为4~5分者患CVD的风险下降28.4%(OR=0.716, 95% CI: 0.592~0.866)。怀孕次数、流产史与生活方式对患CVD的风险存在联合作用,怀孕≥5次时,生活方式得分与患CVD的风险呈负相关。无论是否流产,生活方式得分与患CVD的风险均呈负相关。 结论 农村地区老年女性高血压患者中,怀孕次数较多、有流产史且健康生活方式较少是CVD防控的重点人群,应加强并提升生活方式教育,促进第一级预防的实施。 Abstract:Objective We aimed to explore the relationship between reproductive factors, lifestyle factors, and the risk of cardiovascular disease (CVD) among rural hypertensive women aged 65 and older, with a particular focus on their joint effects. Methods A cluster sampling method was used to conduct face-to-face interviews and physical examinations among elderly female hypertensive patients in a county, Henan Province between July and August 2023. Reproductive factors included the number of pregnancies, live births, and history of miscarriage. Lifestyle factors included sleep, diet, physical activity, passive smoking, and BMI. Logistic regression analysis was employed to assess the impact of reproductive and lifestyle factors, both individually and jointly, on the risk of CVD. Results A total of 9 837 participants were included in the analysis, of whom 3 980 were diagnosed with CVD. Logistic regression analysis revealed that women with ≥5 pregnancies OR a history of miscarriage had a 19.8% (OR=1.198, 95% CI: 1.057-1.359) and 26.1% (OR=1.261, 95% CI: 1.151-1.381) increased risk of developing CVD, respectively. In contrast, those with a lifestyle score of 4-5 had a 28.4% (OR=0.716, 95% CI: 0.592-0.866) reduced risk of developing CVD. A joint effect was observed between the number of pregnancies, history of miscarriage, and lifestyle on the risk of CVD. Specifically, among women with ≥5 pregnancies, a higher lifestyle score was negatively associated with the risk of CVD. Regardless of miscarriage history, a higher lifestyle score was consistently associated with a lower risk of CVD. Conclusions Elderly hypertensive women with a higher number of pregnancies, a history of miscarriage, and unhealthy lifestyles represent a high-risk population for CVD prevention and control. Enhancing health education on healthy lifestyles and promoting primary prevention strategies are essential in reducing the burden of CVD in this vulnerable group. -
Key words:
- Rural areas /
- Reproductive history /
- Lifestyle /
- Cardiovascular diseases
-
表 1 CVD患病率在不同特征组间的比较
Table 1. Comparison of CVD prevalence among different characteristic groups
基本特征Basic characteristics 例数Number of cases① CVD① χ2值value P值value 无No 有Yes 年龄组/岁Age group/years 1.911 0.168 < 72 4 972(50.5) 2 994(51.1) 1 978(49.7) ≥72 4 865(49.5) 2 863(48.9) 2 002(51.3) 民族Nation 6.103 0.014 汉族Han nationality 9 718(98.8) 5 773(98.6) 3 945(99.1) 其他民族Other nationalities 119(1.2) 84(1.4) 35(0.9) 婚姻状况Marital status 0.763 0.683 已婚Married 6 690(68.0) 4 003(68.3) 2 687(67.5) 丧偶Windowed 3 034(30.8) 1 787(30.5) 1 247(31.3) 其他Others 113(1.2) 67(1.2) 46(1.2) 受教育水平Education level 9.166 0.010 未上学Illiteracy 6 019(61.2) 3 549(60.6) 2 470(62.1) 小学Elementary school 2 782(28.3) 1 646(28.1) 1 136(28.5) 初中及以上Junior high school or above 1 036(10.5) 662(11.3) 374(9.4) 家庭年收入/元Average yearly income /yuan 0.629 0.432 ≤30 000 9 188(93.4) 5 467(93.2) 3 727(93.6) >30 000 649(6.6) 396(6.8) 253(6.4) 高血压病程/年Hypertension duration/year 174.066 < 0.001 ≤5 2 928(29.8) 2 037(34.8) 891(22.4) >5 6 909(70.2) 3 820(65.2) 3 089(77.6) 血压控制Blood pressure control 0.203 0.663 差Poor 4 254(43.2) 2 522(43.1) 1 732(43.5) 良好Well 5 583(56.8) 3 335(56.9) 2 248(56.5) 怀孕次数/次Number of pregnancies/times 10.019 0.007 0~2 2 573(26.2) 1 588(27.1) 985(24.8) 3~4 5 115(52.0) 3 040(51.9) 2 075(52.1) ≥5 2 149(21.8) 1 229(21.0) 920(23.1) 活产婴儿数/个Number of live births/piece 5.148 0.076 0~1 374(3.8) 233(4.0) 141(3.5) 2~3 6 231(63.3) 3 748(64.0) 2 483(62.4) ≥4 3 232(32.9) 1 876(32.0) 1 356(34.1) 流产史History of miscarriage 21.195 < 0.001 无No 7 138(72.6) 4 350(74.3) 2 788(70.1) 有Yes 2 699(27.4) 1 507(25.7) 1 192(29.9) 睡眠充足Adequate sleep duration 41.403 < 0.001 否No 3 941(40.1) 2 193(37.4) 1 748(43.9) 是Yes 5 896(59.9) 3 664(62.6) 2 232(56.1) 体力活动充足Adequate physical activity 17.836 < 0.001 否No 1 484(15.1) 810(13.8) 674(16.9) 是Yes 8 353(84.9) 5 047(86.2) 3 306(83.1) 健康饮食Healthy diet 6.008 0.014 否No 9 459(96.2) 5 609(95.8) 3 850(96.7) 是Yes 378(3.8) 248(4.2) 130(3.3) 被动吸烟Passive smoking 6.815 0.010 是No 1 597(16.2) 904(15.4) 693(17.4) 否Yes 8 240(83.8) 4 953(84.6) 3 287(82.6) BMI/(kg·m-2) 9.936 0.019 < 18.5 3 714(37.8) 200(3.4) 126(3.2) 18.5~<24.0 326(3.3) 2 275(38.8) 1 439(36.2) 24.0~<28.0 3 835(39.0) 2 259(38.6) 1 576(39.6) ≥28.0 1 962(19.9) 1 123(19.2) 839(21.0) 生活方式得分/分Lifestyle score/score 20.049 < 0.001 0~<2 524(5.3) 284(4.8) 240(6.0) 2~<4 6 502(66.1) 3 811(65.1) 2 691(67.6) 4~5 2 811(28.6) 1 762(30.1) 1 049(26.4) 注:CVD,心血管病。①以人数(占比/%)表示。
Note: CVD, cardiovascular disease.① Number of people(proportion/%).表 2 生育史、生活方式得分与患CVD风险的关联分析
Table 2. Analysis of the association between reproductive factors, lifestyle score and the risk of CVD
变量Variable 模型1 Model 1① 模型2 Model 2② OR值value (95% CI) P值value OR值value (95% CI) P值value 怀孕次数Number of pregnancies 0~2 1.000 1.000 3~4 1.100(0.999~1.213) 0.053 1.094(0.989~1.210) 0.080 ≥5 1.207(1.074~1.356) 0.002 1.198(1.057~1.359) 0.005 活产婴儿数/个Number of live births/piece 0~1 1.000 1.000 2~3 1.095(0.883~1.358) 0.410 1.080(0.869~1.342) 0.488 ≥4 1.194(0.958~1.489) 0.114 1.159(0.924~1.454) 0.202 流产史History of miscarriage 无No 1.000 1.000 有Yes 1.234(1.128~1.350) < 0.001 1.261(1.151~1.381) < 0.001 生活方式得分/分Lifestyle score/score 0~<2 1.000 1.000 2~<4 0.836(0.699~0.999) 0.049 0.849(0.709~1.018) 0.077 4~5 0.704(0.584~0.850) < 0.001 0.716(0.592~0.866) 0.001 注: CVD,心血管病。
①模型1,未校正模型; ②模型2,在模型1的基础上进一步校正年龄、民族、婚姻状况、受教育水平、家庭年收入、高血压病程、血压控制情况。
Note: CVD, cardiovascular disease.
① Model 1, unadjusted model; ② Model 2, based on model 1, further adjusted for potential confounding factors, including age, nation, marital status, education level, average yearly income, hypertension duration, blood pressure control. -
[1] Vogel B, Acevedo M, Appelman Y, et al. The Lancet women and cardiovascular disease commission: reducing the global burden by 2030 [J]. Lancet, 2021, 397(10292): 2385-2438. DOI: 10.1016/s0140-6736(21)00684-X. [2] Wang C, Yuan Y, Zheng MY, et al. Association of age of onset of hypertension with cardiovascular diseases and mortality [J]. J Am Coll Cardiol, 2020, 75(23): 2921-2930. DOI: 10.1016/j.jacc.2020.04.038. [3] Zhang YB, Chen C, Pan XF, et al. Associations of healthy lifestyle and socioeconomic status with mortality and incident cardiovascular disease: two prospective cohort studies [J]. BMJ, 2021, 373: n604. DOI: 10.1136/bmj.n604. [4] Quenby S, Gallos ID, Dhillon-Smith RK, et al. Miscarriage matters: the epidemiological, physical, psychological, and economic costs of early pregnancy loss [J]. Lancet, 2021, 397(10285): 1658-1667. DOI: 10.1016/s0140-6736(21)00682-6. [5] Wang MM, Zhang JL, Yuan LJ, et al. Miscarriage and stillbirth in relation to risk of cardiovascular diseases: a systematic review and Meta-analysis [J]. Eur J Obstet Gynecol Reprod Biol, 2024, 297: 1-7. DOI: 10.1016/j.ejogrb.2024.03.035. [6] 李子旭, 王霄琼, 江凤, 等. 人工流产对农村女性健康预期寿命的影响研究[J]. 中华疾病控制杂志, 2024, 28(10): 1130-1136. DOI: 10.16462/j.cnki.zhjbkz.2024.10.003.Li ZX, Wang XQ, Jiang F, et al. Study on the effect of induced abortion on healthy life expectancy of rural women [J]. Chin J Dis Control Prev, 2024, 28(10): 1130-1136. DOI: 10.16462/j.cnki.zhjbkz.2024.10.003. [7] Xing ZL, Alman AC, Kirby RS. Kirby. Parity and risk of cardiovascular disease in women over 45 years in the United States: national health and nutrition examination survey 2007-2018 [J]. J Womens Health, 2022, 31(10): 1459-1466. DOI: 10.1089/jwh.2021.0650. [8] Chen TH, Wu JW, Pan QY, et al. The association of female reproductive factors with history of cardiovascular disease: a large cross-sectional study [J]. BMC Public Health, 2024, 24(1): 1616. DOI: 10.1186/s12889-024-19130-4. [9] Guasch-Ferré M, Li YP, Bhupathiraju SN, et al. Healthy lifestyle score including sleep duration and cardiovascular disease risk [J]. Am J Prev Med, 2022, 63(1): 33-42. DOI: 10.1016/j.amepre.2022.01.027. [10] Wang SS, Lay S, Yu HN, et al. Dietary guidelines for Chinese residents (2016): comments and comparisons [J]. J Zhejiang Univ Sci B, 2016, 17(9): 649-656. DOI: 10.1631/jzus.B1600341. [11] Bull FC, Al-Ansari SS, Biddle S, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour [J]. Br J Sports Med, 2020, 54(24): 1451-1462. DOI: 10.1136/bjsports-2020-102955. [12] 余新艳, 苏鹏, 袁晓静, 等. 基层老年慢性病患者心血管疾病综合发生风险的影响因素研究[J]. 中国全科医学, 2024, 27(10): 1186-1193, 1200. DOI: 10.12114/j.issn.1007-9572.2023.0604.Yu XY, Su P, Yuan XJ, et al. A study on the factors influencing the comprehensive risk of cardiovascular disease in elderly patients with chronic disease in primary care [J]. Chin Gen Pract, 2024, 27(10): 1186-1193, 1200. DOI: 10.12114/j.issn.1007-9572.2023.0604. [13] Liang C, Chung HF, Dobson AJ, et al. Infertility, recurrent pregnancy loss, and risk of stroke: pooled analysis of individual patient data of 618 851 women [J]. BMJ, 2022, 377: e070603. DOI: 10.1136/bmj-2022-070603. [14] Wang YX, Mínguez-Alarcón L, Gaskins AJ, et al. Pregnancy loss and risk of cardiovascular disease: the nurses′ health study Ⅱ [J]. Eur Heart J, 2022, 43(3): 190-199. DOI: 10.1093/eurheartj/ehab737. [15] Yang XY, Fan QL, Shen C, et al. Pregnancy loss was associated with the increased risk of cardiovascular diseases in middle-aged women: evidence from the China health and retirement longitudinal study [J]. Glob Heart, 2025, 20(1): 1. DOI: 10.5334/gh.1386. [16] Petersen MMBS, Hartwig TS, Nielsen HS. Pregnancy loss and cardiovascular diseases in women: recent findings and potential mechanisms [J]. Curr Atheroscler Rep, 2022, 24(12): 889-899. DOI: 10.1007/s11883-022-01065-z. [17] Wu J, Feng YF, Zhao YY, et al. Lifestyle behaviors and risk of cardiovascular disease and prognosis among individuals with cardiovascular disease: a systematic review and Meta-analysis of 71 prospective cohort studies [J]. Int J Behav Nutr Phys Act, 2024, 21(1): 42. DOI: 10.1186/s12966-024-01586-7. [18] Zhang YB, Pan XF, Lu Q, et al. Association of combined healthy lifestyles with cardiovascular disease and mortality of patients with diabetes: an international multicohort study [J]. Mayo Clin Proc, 2023, 98(1): 60-74. DOI: 10.1016/j.mayocp.2022.08.012. [19] Peila RT, Xue XN, Shadyab AH, et al. Association between the healthy lifestyle index and risk of multimorbidity in the women′s health initiative [J]. J Gerontol A Biol Sci Med Sci, 2023, 78(12): 2282-2293. DOI: 10.1093/gerona/glad170. [20] 李焕, 张继娜, 马云霞, 等. 农村老年高血压患者心血管疾病风险感知及对自我管理的影响[J]. 护理学杂志, 2023, 38(19): 12-15, 33. DOI: 10.3870/j.issn.1001-4152.2023.19.012.Li H, Zhang JN, Ma YX, et al. Risk perception of cardiovascular disease and its impact on self-management in rural elderly patients with hypertension [J]. Journal of Nursing Science, 2023, 38(19): 12-15, 33. DOI:10.3870/j.issn.1001-4152. 2023.19. 012. -





 下载:
下载: