The association between different metabolic obesity phenotypes and gallstone disease risk
-
摘要:
目的 通过开展全国多中心横断面研究,探讨不同代谢肥胖表型与人群患胆结石风险的关联性。 方法 连续纳入2015―2020年在重庆市和北京市4所三级甲等医院健康体检的研究对象,采用多因素logistic回归分析,比较代谢健康非肥胖(metabolically healthy non-obese, MHNO)、代谢健康型肥胖(metabolically healthy obesity, MHO)、代谢异常型非肥胖(metabolically unhealthy non-obese, MUNO)、代谢异常型肥胖(metabolically unhealthy obesity, MUO)与人群患胆结石风险的关联性,再采用随机效应模型对4个中心的结果进行Meta分析合并。 结果 共招募522 958名研究对象,胆结石总患病率为7.5%。MUO、MUNO、MHO和MHNO组胆结石患病率分别为9.4%、8.3%、6.5%和4.2%,组间差异均有统计学意义(均P < 0.05)。与MHNO组相比,MHO组患胆结石的风险增加了35.8%(合并OR=1.358, 95% CI: 1.213~1.520, P < 0.001);MUNO组患胆结石的风险增加了34.3%(合并OR=1.343, 95% CI: 1.211~1.489, P < 0.001);MUO组患胆结石的风险增加了48.9%(合并OR=1.489, 95% CI: 1.221~1.817, P < 0.001)。亚组分析显示,在不同性别和年龄组中,代谢肥胖表型与人群患胆结石风险的关联性差异均无统计学意义(均P>0.05)。 结论 无论是否伴随代谢异常,肥胖群体均会增加患胆结石的风险。未来应对肥胖群体,尤其是伴有代谢异常者,进行早期筛查与干预,以减少胆结石的疾病负担。 Abstract:Objective This study aimed to investigate the association between different metabolic obesity phenotypes and the risk of gallstone disease through a nationwide multicenter cross-sectional study. Methods Participants who underwent health check-ups in four tertiary hospitals in Chongqing and Beijing from 2015 to 2020 were consecutively enrolled. A multivariate logistic regression analysis was used to compare the risk of gallstone disease among metabolically healthy non-obese (MHNO), metabolically healthy obese (MHO), metabolically unhealthy non-obese (MUNO), and metabolically unhealthy obese (MUO) groups. Finally, a random-effects model was employed to pool the Results from the four centers through meta-analysis. Results A total of 522 958 participants were recruited in this study, with an overall prevalence of gallstone disease of 7.5%. The prevalence of gallstone disease in the MUO, MUNO, MHO, and MHNO groups was 9.4%, 8.3%, 6.5%, and 4.2%, respectively, with statistically significant differences among the groups(all P < 0.05). Compared with the MHNO group, the risk of gallstone disease in the MHO group increased significantly by 35.8%(pooled OR=1.358; 95% CI: 1.213-1.520; P < 0.001); in the MUNO group, it increased by 34.3% (pooled OR=1.343; 95% CI: 1.211-1.489; P < 0.001); and in the MUO group, it increased by 48.9% (pooled OR=1.489; 95% CI: 1.221-1.817; P < 0.001). Subgroup analysis showed no significant differences in the association between metabolic obesity phenotypes and the risk of gallstone disease across different genders and age groups (all P>0.05). Conclusions Obesity, whether accompanied by metabolic abnormalities or not, significantly increases the risk of gallstone disease. Future efforts should focus on early screening and intervention for obese individuals, especially those with metabolic abnormalities, to reduce the burden of gallstone disease. -
Key words:
- Gallstones /
- Metabolic syndrome /
- Obesity
-
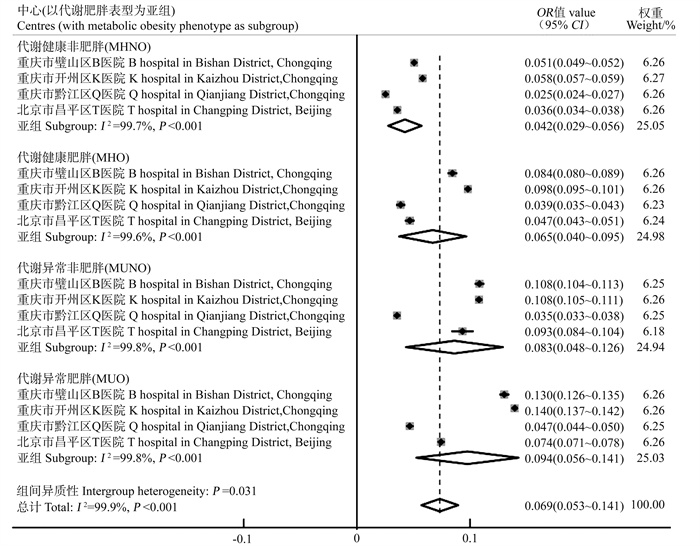
图 1 不同代谢肥胖表型人群胆结石患病率森林图
MHNO:代谢健康非肥胖;MHO:代谢健康型肥胖;MUNO:代谢异常型非肥胖;MUO:代谢异常型肥胖;I2: 异质性指数。
Figure 1. Forest plot of gallstone prevalence for different metabolic obesity phenotypes
MHNO: metabolically healthy non-obese; MHO: metabolically healthy obesity; MUNO: metabolically unhealthy non-obese; MUO: metabolically unhealthy obesity; I2: I-squared statistic.
表 1 各中心研究对象基线特征
Table 1. Baseline characteristics of study population by centre
变量Variable 重庆市璧山区B医院B hospital in Bishan District, Chongqing (n= 131 478) 重庆开州区K医院K hospital in Kaizhou District, Chongqing (n= 250 947) 胆结石Gallstone① 非胆结石Non-gallstone① χ2/Z值value P值value 胆结石Gallstone① 非胆结石Non-gallstone① χ2/Z值value P值value 总人群Total 10 267 121 211 22 828 228 119 年龄/岁Age /years 52.0(43.0, 61.0) 39.0(31.0, 51.0) -73.585 < 0.001 52.0(45.0, 60.0) 44.0(35.0, 52.0) -86.981 < 0.001 性别Gender 107.681 < 0.001 896.076 < 0.001 男性Male 5 481(53.4) 71 084(58.6) 10 201(44.7) 125 560(55.0) 女性Female 4 786(46.6) 50 127(41.4) 12 627(55.3) 102 559(45.0) BMI /(kg·m-2) 24.4(22.4, 26.5) 23.2(21.0, 25.4) -37.636 < 0.001 25.1(23.0, 27.2) 23.8(21.6, 26.1) -54.202 < 0.001 DBP /mmHg 77.0(70.0, 86.0) 73.0(67.0, 82.0) -35.807 < 0.001 79.0(71.0, 88.0) 76.0(69.0, 85.0) -45.536 < 0.001 SBP /mmHg 128.0(116.0, 141.0) 121.0(111.0, 133.0) -29.929 < 0.001 127.0(115.0, 141.0) 121.0(111.0, 134.0) -28.810 < 0.001 FBG /(mmol·L-1) 5.4(5.1, 6.0) 5.2(4.9, 5.6) -36.962 < 0.001 5.5(5.2, 6.1) 5.3(5.0, 5.7) -51.989 < 0.001 TC /(mmol·L-1) 5.0(4.4, 5.6) 4.8(4.2, 5.6) -14.222 < 0.001 5.1(4.5, 5.8) 5.0(4.4, 5.6) -12.518 < 0.001 TG /(mmol·L-1) 1.5(1.0, 2.2) 1.2(0.9, 1.9) -30.658 < 0.001 1.6(1.1, 2.3) 1.3(0.9, 2.0) -39.606 < 0.001 LDL-C /(mmol·L-1) 3.0(2.5, 3.6) 2.9(2.4, 3.4) -14.683 < 0.001 2.6(2.2, 3.1) 2.5(2.2, 3.0) -17.499 < 0.001 HDL-C /(mmol·L-1) 1.3(1.1, 1.6) 1.4(1.2, 1.6) -12.517 < 0.001 1.3(1.1, 1.5) 1.4(1.2, 1.6) -16.994 < 0.001 AST /(U·L-1) 22.0(18.0, 27.0) 21.0(17.0, 26.0) -10.330 < 0.001 24.0(20.0, 30.0) 23.0(19.0, 29.0) -11.624 < 0.001 ALT /(U·L-1) 22.0(16.0, 33.0) 21.0(14.0, 32.0) -11.678 < 0.001 23.0(16.5, 34.0) 21.0(15.0, 32.0) -17.114 < 0.001 GGT /(U·L-1) 27.0(18.0, 45.0) 24.0(16.0, 40.0) -22.105 < 0.001 26.0(17.0, 42.0) 22.0(15.0, 37.0) -13.370 < 0.001 TBIL /(μmol·L-1) 12.8(10.3, 16.2) 12.7(10.1, 16.1) -3.252 0.001 ― ― ― ― SUA /(μmol·L-1) 341.0(281.0, 407.0) 339.0(275.0, 408.0) -2.802 < 0.001 333.8(277.7, 397.79) 333.6(274.3, 399.5) -1.358 0.174 BUN /(mmol/L-1) 5.1(4.3, 6.1) 5.0(4.2, 5.9) -13.265 < 0.001 5.2(4.3, 6.2) 5.1(4.3, 6.1) -11.138 < 0.001 脂肪肝Fatty liver 4 262(41.5) 31 551(26.0) 1 144.693 < 0.001 9 518(41.7) 61 563(27.0) 1 144.693 < 0.001 肾结石Kidney stone 559(5.4) 5 205(4.3) 29.887 < 0.001 854(3.7) 7 585(3.3) 11.051 0.001 胆囊息肉Gallbladder polyp 264(2.6) 10 504(8.7) 467.565 < 0.001 493(2.2) 21 920(9.6) 1 415.801 < 0.001 代谢肥胖表型Metabolic obesity phenotype 1 897.543 < 0.001 3 338.360 < 0.001 MHNO 3 589(35.0) 67 338(55.6) 6 703(29.4) 108 631(47.6) MHO 1 377(13.4) 14 930(12.3) 3 636(15.9) 33 394(14.6) MUNO 2 294(22.3) 18 878(15.6) 4 351(19.1) 35 951(15.8) MUO 3 007(29.3) 20 065(16.6) 8 138(35.6) 50 143(22.0) 变量Variable 重庆黔江区Q医院Q hospital in Qianjiang District, Chongqing (n=70 156) 北京市昌平区T医院T hospital in Changping District, Beijing (n=70 377) 胆结石Gallstone① 非胆结石Non-gallstone① χ2/Z值value P值value 胆结石Gallstone① 非胆结石Non-gallstone① χ2/Z值value P值value 总人群Total 2 398 67 758 3 844 66 533 年龄/岁Age /years 52.0(44.0, 61.0) 33.0(22.0, 46.0) -48.577 < 0.001 55.0(45.0, 68.0) 42.0(33.0, 52.0) -50.202 < 0.001 性别Gender 73.134 < 0.001 2.266 0.132 男性Male 1 102(46.0) 37 134(54.8) 2 275(59.2) 40 189(60.4) 女性Female 1 296(54.0) 30 624(45.2) 1 569(40.8) 26 344(39.6) BMI /(kg·m-2) 24.6(22.5, 26.8) 23.7(21.5, 26.0) -13.539 < 0.001 26.0(23.9, 28.2) 25.0(22.5, 27.4) -17.302 < 0.001 DBP /mmHg 79.0(71.0, 86.5) 76.1(69.0, 84.0) -14.680 < 0.001 76.0(70.0, 82.0) 74.0(67.0, 80.0) -10.392 < 0.001 SBP /mmHg 129.0(117.0, 141.0) 124.0(113.0, 135.0) -10.120 < 0.001 125.0(115.0, 137.0) 119.0(110.0, 130.0) -22.282 < 0.001 FBG /(mmol·L-1) 5.3(4.9, 5.9) 5.2(4.7, 5.7) -12.720 < 0.001 5.5(5.1, 6.1) 5.2(4.9, 5.6) -23.046 < 0.001 TC /(mmol·L-1) 5.0(4.4, 5.6) 4.9(4.3, 5.5) -4.784 < 0.001 4.9(4.2, 5.5) 4.7(4.2, 5.4) -7.696 < 0.001 TG /(mmol·L-1) 1.8(1.2, 2.5) 1.7(1.1, 2.6) -4.878 < 0.001 1.4(1.0, 2.0) 1.2(0.8, 1.9) -11.356 < 0.001 LDL-C /(mmol·L-1) 2.7(2.2, 3.2) 2.6(2.1, 3.1) -4.662 < 0.001 3.0(2.5, 3.6) 2.9(2.4, 3.5) -6.902 < 0.001 HDL-C /(mmol·L-1) 1.3(1.1, 1.5) 1.4(1.1, 1.6) -6.588 < 0.001 1.3(1.1, 1.5) 1.3(1.1, 1.5) -5.345 < 0.001 AST /(U·L-1) 23.0(16.2, 33.9) 19.4(13.0, 32.0) -12.036 < 0.001 20.5(17.1, 24.9) 20.0(17.0, 24.2) -5.070 < 0.001 ALT /(U·L-1) 23.0(19.0, 28.5) 22.1(18.0, 28.2) -5.374 < 0.001 19.6(14.5, 27.8) 19.0(13.5, 28.0) -4.055 < 0.001 TBIL /(μmol·L-1) 13.3(10.6, 16.9) 13.6(10.4, 17.7) -1.730 0.084 ― ― ― ― SUA /(μmol·L-1) ― ― ― ― 337.4(281.4, 397.0) 326.0(267.0, 389.0) -7.803 < 0.001 脂肪肝Fatty liver 1 056(44.0) 8 003(11.8) 2 138.824 < 0.001 9 518(41.7) 61 563(27.0) 186.847 < 0.001 肾结石Kidney stone 61(2.5) 659(1.0) 56.289 < 0.001 279(7.3) 2 152(3.2) 176.412 < 0.001 高血压Hypertension ― ― ― ― 1 773(46.1) 17 108(25.7) 771.170 < 0.001 糖尿病Diabetes ― ― ― ― 755(19.6) 5 847(8.8) 503.518 < 0.001 代谢肥胖表型Metabolic obesity phenotype 151.281 < 0.001 510.085 < 0.001 MHNO 738(30.8) 28 426(42.0) 1 124(29.7) 30 251(45.5) MHO 338(14.1) 8 402(12.4) 444(11.6) 9 055(13.6) MUNO 581(24.2) 15 811(23.3) 317(8.2) 3 078(4.6) MUO 741(30.9) 15 119(22.3) 1 941(50.5) 24 149(36.3) 注:DBP,舒张压;SBP,收缩压;FBG,空腹血糖;TC,总胆固醇;LDL-C,低密度脂蛋白胆固醇;HDL-C,高密度脂蛋白胆固醇;TG,三酰甘油;AST,天冬氨酸氨基转移酶;ALT,γ-谷氨酰转移酶;GGT,丙氨酸氨基转移酶;TBIL,总胆红素;SUA,血清尿酸;BUN,尿素氮;MHNO,代谢健康非肥胖;MHO,代谢健康型肥胖;MUNO,代谢异常型非肥胖;MUO,代谢异常型肥胖;“―”表示该中心缺乏该数据。
①以人数(占比/%)或M(P25, P75)表示。
Note: DBP, diastolic blood pressure; SBP, systolic blood pressure; FBG, fasting blood glucose; TC, total cholesterol; LDL-C, low-density lipoprotein cholesterol; HDL-C, high-density lipoprotein cholesterol; TG, triglycerides; AST, aspartate aminotransferase; ALT, alanine aminotransferase; GGT, gamma-glutamyl transferase; TBIL, total bilirubin; SUA, serum uric acid; BUN, blood urea nitrogen; MHNO, metabolically healthy non-obese; MHO, metabolically healthy obesity; MUNO, metabolically unhealthy non-obese; MUO, metabolically unhealthy obesity; "―" indicates that the center lacks the data.
① Number of people(proportion/%) or M(P25, P75).表 2 胆结石与代谢肥胖表型的相关性多因素logistic回归分析
Table 2. Multifactorial logistic regression analysis of the correlation between gallstones and metabolic obesity phenotype
变量Variable 重庆市璧山区B医院B hospital in Bishan District, Chongqing 重庆市开州区K医院K hospital in Kaizhou District, Chongqing 重庆市黔江区Q医院Q hospital in Qianjiang District, Chongqing 北京市昌平区T医院T hospital in Changping District, Beijing OR值value (95% CI) P值value OR值value (95% CI) P值value OR值value (95% CI) P值value OR值value (95% CI) P值value 总计Total MHNO 1.000 1.000 1.000 1.000 MHO 1.469(1.370~1.576) < 0.001 1.526(1.458~1.596) < 0.001 1.169(1.018~1.343) 0.027 1.222(1.086~1.376) 0.001 MUNO 1.454(1.369~1.545) < 0.001 1.435(1.375~1.498) < 0.001 1.082(0.963~1.215) 0.187 1.385(1.208~1.587) < 0.001 MUO 1.781(1.670~1.899) < 0.001 1.828(1.752~1.907) < 0.001 1.063(0.946~1.195) 0.306 1.388(1.268~1.519) < 0.001 性别Gender 男性Male MHNO 1.000 1.000 1.000 1.000 MHO 1.488(1.356~1.632) < 0.001 1.553(1.450~1.664) < 0.001 1.146(0.934~1.407) 0.191 1.266(1.089~1.471) 0.002 MUNO 1.402(1.287~1.527) < 0.001 1.370(1.280~1.466) < 0.001 1.186(0.987~1.425) 0.069 1.374(1.146~1.648) 0.001 MUO 1.831(1.683~1.992) < 0.001 1.797(1.686~1.915) < 0.001 1.267(1.068~1.504) 0.007 1.455(1.307~1.619) < 0.001 性别Gender 女性Female MHNO 1.000 1.000 1.000 1.000 MHO 1.465(1.313~1.634) < 0.001 1.498(1.410~1.592) < 0.001 1.241(1.025~1.502) 0.027 1.395(1.162~1.674) < 0.001 MUNO 1.488(1.365~1.623) < 0.001 1.474(1.394~1.559) < 0.001 1.007(0.864~1.173) 0.931 1.533(1.251~1.880) < 0.001 MUO 1.676(1.512~1.858) < 0.001 1.853(1.747~1.964) < 0.001 0.874(0.740~1.033) 0.114 1.773(1.569~2.004) < 0.001 年龄组/岁Age group/years ≤40 MHNO 1.000 1.000 1.000 1.000 MHO 1.919(1.664~2.212) < 0.001 1.885(1.695~2.097) < 0.001 1.121(0.838~1.500) 0.442 1.740(1.347~2.248) < 0.001 MUNO 1.645(1.417~1.910) < 0.001 1.606(1.424~1.810) < 0.001 0.789(0.603~1.031) 0.083 1.904(1.135~3.194) 0.015 MUO 2.317(1.986~2.704) < 0.001 2.011(1.787~2.264) < 0.001 0.951(0.726~1.245) 0.715 1.551(1.204~1.998) 0.001 >40~<60 MHNO 1.000 1.000 1.000 1.000 MHO 1.317(1.194~1.452) < 0.001 1.460(1.380~1.544) < 0.001 1.118(0.927~1.349) 0.243 1.118(0.944~1.324) 0.198 MUNO 1.367(1.257~1.488) < 0.001 1.405(1.331~1.483) < 0.001 1.174(1.005~1.371) 0.043 1.481(1.196 ~1.835) < 0.001 MUO 1.688(1.544~1.846) < 0.001 1.768(1.677~1.865) < 0.001 1.049(0.897~1.226) 0.552 1.557(1.369~1.772) < 0.001 ≥60 MHNO 1.000 1.000 1.000 1.000 MHO 1.510(1.307~1.746) < 0.001 1.465(1.313~1.634) < 0.001 1.334(0.997~1.784) 0.052 1.189(0.946~1.494) 0.138 MUNO 1.486(1.333~1.656) < 0.001 1.395(1.277~1.525) < 0.001 1.166(0.913~1.489) 0.220 1.153(0.952~1.396) 0.146 MUO 1.676(1.491~1.885) < 0.001 1.831(1.672~2.006) < 0.001 1.212(0.954~1.540) 0.115 1.119(0.967~1.295) 0.130 注:MHNO,代谢健康非肥胖;MHO,代谢健康型肥胖;MUNO,代谢异常型非肥胖;MUO,代谢异常型肥胖。
Note: MHNO, metabolically healthy non-obese; MHO, metabolically healthy obesity; MUNO, metabolically unhealthy non-obese; MUO, metabolically unhealthy obesity. -
[1] Wang X, Yu WQ, Jiang GH, et al. Global epidemiology of gallstones in the 21st century: a systematic review and Meta-analysis [J]. Clin Gastroenterol Hepatol, 2024, 22(8): 1586-1595. DOI: 10.1016/j.cgh.2024.01.051. [2] Lammert F, Wittenburg H. Gallstones: prevention, diagnosis, and treatment [J]. Semin Liver Dis, 2024, 44(3): 394-404. DOI: 10.1055/a-2378-9025. [3] Ratheesh R, Ulrich MT, Ghozy S, et al. The association between diabetes and gallstones: a nationwide population-based cohort study [J]. Prz Gastroenterol, 2023, 18(3): 292-299. DOI: 10.5114/pg.2023.131395. [4] Luo X, Yang WS, Joshi AD, et al. Gallstones and risk of cancers of the liver, biliary tract and pancreas: a prospective study within two U.S. cohorts [J]. Br J Cancer, 2022, 127(6): 1069-1075. DOI: 10.1038/s41416-022-01877-5. [5] Yuan S, Gill D, Giovannucci EL, et al. Obesity, type 2 diabetes, lifestyle factors, and risk of gallstone disease: a Mendelian randomization investigation [J]. Clin Gastroenterol Hepatol, 2022, 20(3): e529-e537. DOI: 10.1016/j.cgh.2020.12.034. [6] BLüHER M. Metabolically Healthy Obesity [J]. Endocrine reviews, 2020, 41(3). DOI: 10.1210/endrev/bnaa004. [7] Janota O, Mantovani M, Kwiendacz H, et al. Metabolically "extremely unhealthy" obese and non-obese people with diabetes and the risk of cardiovascular adverse events: the Silesia diabetes - heart project [J]. Cardiovasc Diabetol, 2024, 23(1): 326. DOI: 10.1186/s12933-024-02420-x. [8] Stefan N. Causes, consequences, and treatment of metabolically unhealthy fat distribution [J]. Lancet Diabetes Endocrinol, 2020, 8(7): 616-627. DOI: 10.1016/S2213-8587(20)30110-8. [9] Dvo r ˇ ák K. Diagnostic methods of fatty liver diseases [J]. Cas Lek Cesk, 2022, 161(2): 57-60. [10] Thongprayoon C, Krambeck AE, Rule AD. Determining the true burden of kidney stone disease [J]. Nat Rev Nephrol, 2020, 16(12): 736-746. DOI: 10.1038/s41581-020-0320-7. [11] Kamaya A, Fung C, Szpakowski JL, et al. Management of incidentally detected gallbladder polyps: society of radiologists in ultrasound consensus conference recommendations [J]. Radiology, 2022, 305(2): 277-289. DOI: 10.1148/radiol.213079. [12] WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies [J]. Lancet, 2004, 363(9403): 157-163. DOI: 10.1016/S0140-6736(03)15268-3. [13] Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive summary of the third report of the national cholesterol education program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel Ⅲ) [J]. JAMA, 2001, 285(19): 2486-2497. DOI: 10.1001/jama.285.19.2486. [14] Lin L, Zhang J, Jiang L, et al. Transition of metabolic phenotypes and risk of subclinical atherosclerosis according to BMI: a prospective study [J]. Diabetologia, 2020, 63(7): 1312-1323. DOI: 10.1007/s00125-020-05116-5. [15] Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of observational studies in epidemiology (MOOSE) group [J]. JAMA, 2000, 283(15): 2008-2012. DOI: 10.1001/jama.283.15.2008. [16] Zhang JL, Chen LL, Shen KQ, et al. Association between metabolically healthy overweight/obesity and gallstones in Chinese adults [J]. Nutr Metab, 2023, 20(1): 20. DOI: 10.1186/s12986-023-00741-4. [17] Man S, Gao YX, Lyu J, et al. Metabolically healthy obesity was significantly associated with increased risk of gallstones [J]. Eur J Endocrinol, 2022, 186(2): 275-283. DOI: 10.1530/EJE-21-0802. [18] Su PY, Hsu YC, Cheng YF, et al. Strong association between metabolically-abnormal obesity and gallstone disease in adults under 50 years [J]. BMC Gastroenterol, 2019, 19(1): 117. DOI: 10.1186/s12876-019-1032-y. [19] Unalp-Arida A, Ruhl CE. Increasing gallstone disease prevalence and associations with gallbladder and biliary tract mortality in the US [J]. Hepatology, 2023, 77(6): 1882-1895. DOI: 10.1097/HEP.0000000000000264. [20] Lee KX, Quek KF, Ramadas A. Dietary and lifestyle risk factors of obesity among young adults: a scoping review of observational studies [J]. Curr Nutr Rep, 2023, 12(4): 733-743. DOI: 10.1007/s13668-023-00513-9. [21] Takei A, Nagashima S, Takei S, et al. Myeloid HMG-CoA reductase determines adipose tissue inflammation, insulin resistance, and hepatic steatosis in diet-induced obese mice [J]. Diabetes, 2020, 69(2): 158-164. DOI: 10.2337/db19-0076. [22] DeForest N, Wang YQ, Zhu ZY, et al. Genome-wide discovery and integrative genomic characterization of insulin resistance loci using serum triglycerides to HDL-cholesterol ratio as a proxy [J]. Nat Commun, 2024, 15(1): 8068. DOI: 10.1038/s41467-024-52105-y. [23] Kubica K, Balbus J. A computer study of the risk of cholesterol gallstone associated with obesity and normal weight [J]. Sci Rep, 2021, 11(1): 8868. DOI: 10.1038/s41598-021-88249-w. [24] Li Y, Onodera T, Scherer PE. Adiponectin [J]. Trends Endocrinol Metab, 2024, 35(7): 674-675. DOI: 10.1016/j.tem.2024.05.004. [25] Yu JJ, Meng ZA, Liu XX, et al. Lipopolysaccharide in bile promotes the neutrophil extracellular traps-induced gallstone formation by activating the gallbladder immune barrier [J]. Immunotargets Ther, 2024, 13: 789-803. DOI: 10.2147/ITT.S495095. -





 下载:
下载: