-
摘要:
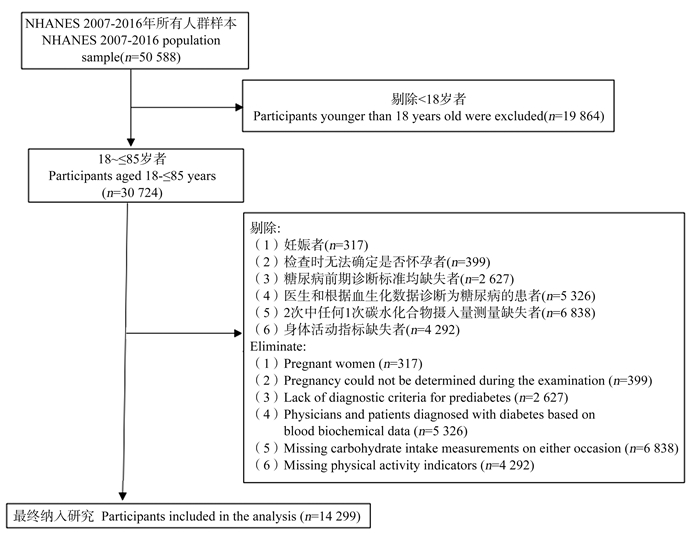
目的 探讨每日碳水化合物摄入量与糖尿病前期患病的关系,为糖尿病前期形成提供证据。 方法 基于美国健康与营养调查2007―2016年数据,纳入与本研究相关且关键指标无缺失的14 299名研究对象。采用非参数协变量均衡广义倾向性评分方法均衡已测得的混杂因素,通过限制性立方样条探究二者关系。 结果 研究人群中位年龄为43岁,糖尿病前期患病率为39.28%。在调整混杂因素后,碳水化合物摄入量与糖尿病前期患病呈非线性关系(P非线性 < 0.001)。与每日摄入量为243.21 g相比,随着碳水化合物摄入量的增加,糖尿病前期的患病风险逐渐升高(OR值逐渐上升)。在高、中和低水平活动人群中,与每日碳水化合物摄入量分别为350.66 g、335.80 g、152.22 g相比,随着碳水化合物摄入量的增加,糖尿病前期的患病风险逐渐升高(OR值逐渐上升)。 结论 碳水化合物摄入量与糖尿病前期患病呈非线性关系,每日摄入超过约240 g的碳水化合物可能是糖尿病前期患病的危险因素。且身体活动水平下降,增加糖尿病前期患病风险的碳水化合物摄入量也会降低。 -
关键词:
- 糖尿病前期 /
- 碳水化合物摄入量 /
- 非参数协变量均衡广义倾向性评分法 /
- 限制性立方样条
Abstract:Objective This study aims to investigate the relationship between daily carbohydrate intake and the prevalence of prediabetes, and to provide direct evidence for the formation of prediabetes. Methods Based on the data from the National Health and Ntrition Examination Survey from 2007 to 2016, 14 299 research subjects related to this study with no missing key indicators were included. The non-parametric covariate balancing generalized propensity score was used to balance the measured confounding factors, and the restricted cubic spline was adopted to explore the relationship between them. Results The median age of the study population was 43 years old, and the prevalence of prediabetes was 39.28%. After adjusting for confounding factors, there was a nonlinear relationship between carbohydrate intake and prediabetes (Pnonlinear < 0.001). Compared with the daily intake of 243.21 g, the risk of prediabetes increased with the increase of carbohydrate intake (OR value gradually increases). In the high, medium and low levels of activity, the risk of prediabetes was gradually increased with the increase of carbohydrate intake (OR value gradually increases) compared with the daily carbohydrate intake of 350.66 g, 335.80 g and 152.22 g, respectively. Conclusions There is a nonlinear relationship between carbohydrate intake and prediabetes. A daily carbohydrate intake of more than approximately 240 g may be a risk factor for prediabetes. Moreover, the carbohydrate intake associated with elevated prediabetes risk is lower in individuals with reduced physical activity. -
图 2 在不同模型下碳水化合物摄入量与糖尿病前期之间的关系
A:模型1,未调整混杂因素; B:模型2,调整了人口学特征; C:模型3,调整了人口学特征和生活方式; D:模型4,调整了人口学特征、生活方式和体检数据。
Figure 2. Association between carbohydrate intake and prediabetes under different models
A: model 1, unadjusted confounders; B: model 2, adjusted demographic characteristics; C: model 3, adjusted demographic characteristics and lifestyle; D: model 4, adjusted demographic characteristics, lifestyle and physical examination data.
图 3 不同模型的均衡性表现
模型1:未调整混杂因素; 模型2:调整了人口学特征; 模型3:调整了人口学特征和生活方式; 模型4:调整了人口学特征、生活方式和体检数据。
Figure 3. Performance of the balance of the different models
Model 1: unadjusted confounders; Model 2: adjusted demographic characteristics; Model 3: adjusted demographic characteristics and lifestyle; Model 4: adjusted demographic characteristics, lifestyle and physical examination data.
图 5 不同身体活动情况的敏感性分析
A、B、C表示分别在低、中、高身体活动水平人群中使用npCBGPS调整了人口学特征、生活方式和体检数据。
Figure 5. Sensitivity analysis of different physical activity status
A, B, C represent adjustments for demographic characteristics, lifestyle, and physical examination data using npCBGPS in populations with low, medium, and high levels of physical activity, respectively.
表 1 研究对象基线特征
Table 1. Baseline characteristics of the subjects
变量
Variable非糖尿病前期
Non-prediabetic state①(n=8 682)糖尿病前期
Prediabetic state①
(n=5 617)检验统计量
Statistic of testP值
value年龄组/岁Age groups/years 1 349.90 < 0.001 18~ < 45 5 690(65.5) 1 979(35.2) 45~ < 60 1 708(19.7) 1 658(29.5) ≥60 1 284(14.8) 1 980(35.3) 性别Gender 50.83 < 0.001 男Male 4 228(48.7) 3 079(54.8) 女Female 4 454(51.3) 2 538(45.2) 婚姻状况Marital status 63.00 < 0.001 离婚/丧偶/分居/未婚Divorced/widowed/separated/never married 3 887(44.8) 2 137(38.0) 已婚/同居Married/live with partners 4 795(55.2) 3 480(62.0) 受教育程度Education 80.18 < 0.001 高中及以下High school or lower 3 429(39.5) 2 645(47.1) 大学及以上University or higher 5 253(60.5) 2 972(52.9) 种族Race 69.89 < 0.001 墨西哥裔美国人Mexican American 1 206(13.9) 825(14.7) 其他西班牙裔Other Hispanics 852(9.8) 567(10.1) 非西班牙裔白人Non-Hispanic whites 4 168(48.0) 2 394(42.6) 非西班牙裔黑人Non-Hispanic blacks 1 497(17.2) 1 251(22.3) 其他种族(包括多种族) Other races (including multi-racial) 959(11.1) 580(10.3) 家庭收入贫困比Ratio of family income to poverty 9.74 0.008 低Low (< 1) 1 860(21.4) 1 116(19.9) 中Medium (1~4) 4 335(49.9) 2 950(52.5) 高High (>4) 2 487(28.7) 1 551(27.6) 吸烟Smoking 78.18 < 0.001 一生中吸烟 < 100支Lifetime smoking < 100 cigarettes 5 379(62.0) 3 061(54.5) 一生中吸烟≥100支Lifetime smoking ≥100 cigarettes 3 303(38.0) 2 556(45.5) 饮酒Drinking 152.41 < 0.001 近1年未喝过酒Haven't drunk in the past year 1 130(13.0) 1 168(20.8) 近1年喝过酒Have drunk in the past year 7 552(87.0) 4 449(79.2) 蛋白质Protein /(g·d-1) 77.48(58.81, 101.25) 76.96(58.22, 100.36) 24 784 322 0.096 脂肪Fat/(g·d-1) 73.11(52.76, 99.10) 72.81(52.76, 99.10) 24 542 764 0.509 BMI/(kg·m-2) 25.68(22.63, 29.41) 27.96(24.64, 31.93) 18 612 707 < 0.001 碳水化合物Carbohydrate/(g·d-1) 244.95(185.00, 315.56) 239.68(183.01, 311.12) 25 019 315 0.008 身体活动Physical activity/(MET·h·w-1) 20.01 < 0.001 < 1 17(0.2) 27(0.5) 1~48 4 870(56.1) 3 299(58.7) >48 3 795(43.7) 2 291(40.8) 注:①以中位数和四分位数间距M(P25, P75)对定量变量进行统计描述,以频数(构成比)对定性变量进行统计描述。
Note: ① The median and interquartile range M(P25, P75) were used to describe the quantitative variables, and the frequency and constituent ratio n(%) were used to describe the qualitative variable. -
[1] 中华医学会内分泌学分会, 中华医学会糖尿病学分会, 中国医师协会内分泌代谢科医师分会. 中国成人糖尿病前期干预的专家共识(2023版)[J]. 中华糖尿病杂志, 2023, 15(6): 484-494. DOI: 10.3760/cma.j.cn115791-20230509-00188.Chinese Society of Endocrinology, Chinese Diabetes Society, Chinese College of Endocrinology and Metabolism Physicians. Chinese expert consensus on the intervention of prediabetes in Chinese adults (2023 edition)[J]. Chin J Diabetes, 2023, 15 (6): 484-494. DOI: 10.3760/cma.j.cn115791-20230509-00188. [2] Echouffo-Tcheugui JB, Selvin E. Prediabetes and what it means: the epidemiological evidence[J]. Annu Rev Public Health, 2021, 42: 59-77. DOI: 10.1146/annurev-publhealth-090419-102644. [3] Echouffo-Tcheugui JB, Perreault L, Ji LN, et al. Diagnosis and management of prediabetes: a review[J]. JAMA, 2023, 329(14): 1206-1216. DOI: 10.1001/jama.2023.4063. [4] Eid SA, Rumora AE, Beirowski B, et al. New perspectives in diabetic neuropathy[J]. Neuron, 2023, 111(17): 2623-2641. DOI: 10.1016/j.neuron.2023.05.003. [5] Schlesinger S, Neuenschwander M, Barbaresko J, et al. Prediabetes and risk of mortality, diabetes-related complications and comorbidities: umbrella review of Meta-analyses of prospective studies[J]. Diabetologia, 2022, 65(2): 275-285. DOI: 10.1007/s00125-021-05592-3. [6] Aune D, Schlesinger S, Mahamat-Saleh Y, et al. Diabetes mellitus, prediabetes and the risk of Parkinson's disease: a systematic review and Meta-analysis of 15 cohort studies with 29.9 million participants and 86 345 cases[J]. Eur J Epidemiol, 2023, 38(6): 591-604. DOI: 10.1007/s10654-023-00970-0. [7] Shen EJ, Chen X. Prediabetes and the risk of lung cancer incidence and mortality: a Meta-analysis[J]. J Diabetes Investig, 2023, 14(10): 1209-1220. DOI: 10.1111/jdi.14057. [8] van Sloten TT, Sedaghat S, Carnethon MR, et al. Cerebral microvascular complications of type 2 diabetes: stroke, cognitive dysfunction, and depression[J]. Lancet Diabetes Endocrinol, 2020, 8(4): 325-336. DOI: 10.1016/S2213-8587(19)30405-X. [9] Wang LM, Peng W, Zhao ZP, et al. Prevalence and treatment of diabetes in China, 2013-2018[J]. JAMA, 2021, 326(24): 2498-2506. DOI: 10.1001/jama.2021.22208. [10] Rooney MR, Fang M, Ogurtsova K, et al. Global prevalence of prediabetes[J]. Diabetes Care, 2023, 46(7): 1388-1394. DOI: 10.2337/dc22-2376. [11] 鲜圆圆, 高静, 柏丁兮, 等. 中国老年人糖尿病前期患病率的Meta分析[J]. 军事护理, 2022, 39(12): 62-65, 100. DOI: 10.3969/j.issn.2097-1826.2022.12.016.Xian YY, Gao J, Bai DX, et al. Prevalence of prediabetes mellitus among Chinese elderly: a Meta-analysis[J]. Mil Nurs, 2022, 39(12): 62-65, 100. DOI: 10.3969/j.issn.2097-1826.2022.12.016. [12] Gardner CD, Landry MJ, Perelman D, et al. Effect of a ketogenic diet versus Mediterranean diet on glycated hemoglobin in individuals with prediabetes and type 2 diabetes mellitus: the interventional Keto-Med randomized crossover trial[J]. Am J Clin Nutr, 2022, 116(3): 640-652. DOI: 10.1093/ajcn/nqac154. [13] Li L, Shan ZL, Wan ZZ, et al. Associations of lower-carbohydrate and lower-fat diets with mortality among people with prediabetes[J]. Am J Clin Nutr, 2022, 116(1): 206-215. DOI: 10.1093/ajcn/nqac058. [14] 田子星, 赵艾, 张健, 等. 城市女性膳食质量与糖尿病及糖尿病前期患病风险的关联研究[J]. 中华预防医学杂志, 2020, 54(7): 742-746. DOI: 10.3760/cma.j.cn112150-20190730-00609.Tian ZX, Zhao A, Zhang J, et al. Association between diet quality and the risk of diabetes and prediabetes in urban women[J]. Chinese preventive medical journal, 2020, (7): 742-746. DOI: 10.3760/cma.j.cn112150-20190730-00609.cma.J.c.n112150-20190730-00609. [15] 赵惠, 宋鹏坤, 何丽. 不同膳食模式对中老年人群糖尿病前期及糖尿病患病的影响[J]. 中国慢性病预防与控制, 2020, 28(3): 182-186. DOI: 10.16386/j.cjpccd.issn.1004-6194.2020.03.005.Zhao H, Song PK, He L. Influence of different dietary patterns on prevalence of prediabetes and diabetes among middle-aged and elderly people[J]. Chin J Prev Control Chronic Dis, 2020, 28(3): 182-186. DOI: 10.16386/j.cjpccd.issn.1004-6194.2020.03.005. [16] Zhang JL, Zhang AH. Relationships between serum Klotho concentrations and cognitive performance among older chronic kidney disease patients with albuminuria in NHANES 2011-2014[J]. Front Endocrinol (Lausanne), 2023, 14: 1215977. DOI: 10.3389/fendo.2023.1215977. [17] ElSayed NA, Aleppo G, Aroda VR, et al. 2. classification and diagnosis of diabetes: standards of care in diabetes-2023[J]. Diabetes Care, 2023, 46(Suppl 1): S19-S40. DOI: 10.2337/dc23-S002. [18] 樊萌语, 吕筠, 何平平. 国际体力活动问卷中体力活动水平的计算方法[J]. 中华流行病学杂志, 2014, 35(8): 961-964. DOI: 10.3760/cma.j.issn.0254-6450.2014.08.019.Fan MY, Lyu Y, He PP. Chinese guidelines for data processing and analysis concerning the international physical activity questionnaire[J]. Chin J Epidemiol, 2014, 35(8): 961-964. DOI: 10.3760/cma.j.issn.0254-6450.2014.08.019. [19] Pelgrims I, Devleesschauwer B, Vandevijvere S, et al. Using random-forest multiple imputation to address bias of self-reported anthropometric measures, hypertension and hypercholesterolemia in the Belgian health interview survey[J]. BMC Med Res Methodol, 2023, 23(1): 69. DOI: 10.1186/s12874-023-01892-x. [20] Fong C, Hazlett C, Imai K. Covariate balancing propensity score for a continuous treatment: application to the efficacy of political advertisements[J]. Ann Appl Stat, 2018, 12(1): 156-177. DOI: 10.1214/17-aoas1101. [21] Sack DE, Shepherd BE, Audet CM, et al. Inverse probability weights for quasicontinuous ordinal exposures with a binary outcome: method comparison and case study[J]. Am J Epidemiol, 2023, 192(7): 1192-1206. DOI: 10.1093/aje/kwad085. [22] Wu LD, Shi Y, Kong CH, et al. Dietary inflammatory index and its association with the prevalence of coronary heart disease among 45 306 US adults[J]. Nutrients, 2022, 14(21): 4553. DOI: 10.3390/nu14214553. [23] Alves R, Perelman J, Chang K, et al. Environmental impact of dietary patterns in 10 European countries; a cross-sectional analysis of nationally representative dietary surveys[J]. Eur J Public Health, 2024, 34(5): 992-1000. DOI: 10.1093/eurpub/ckae088. [24] Desbouys L, Méjean C, De Henauw S, et al. Socio-economic and cultural disparities in diet among adolescents and young adults: a systematic review[J]. Public Health Nutr, 2020, 23(5): 843-860. DOI: 10.1017/S1368980019002362. [25] Ness A. Diet, nutrition and the prevention of chronic diseases. WHO technical report series 916. report of a joint WHO/FSA expert consultation[J]. Int J Epidemiol, 2004, 33(4): 914-915. DOI: 10.1093/ije/dyh209. [26] Lee CL, Liu WJ, Wang JS. Associations of low-carbohydrate and low-fat intakes with all-cause mortality in subjects with prediabetes with and without insulin resistance[J]. Clin Nutr, 2021, 40(5): 3601-3607. DOI: 10.1016/j.clnu.2020.12.019. [27] 周美岑. 线粒体及其调控基因在糖脂异常发生机制中的作用[D]. 北京: 北京协和医学院, 2016.Zhou MC. The role of mitochondria and their regulatory genes in the pathogenesis of glucose and lipid abnormalities[D]. Beijing: Peking Union Medical College, 2016. [28] 江美玲. 2型糖尿病及其前期状态人群肠道菌群特征分析[D]. 广州: 南方医科大学, 2013.Jiang ML. Characteristics of intestinal flora in people with type 2 diabetes and prediabetes[D]. Guangzhou: Southern Medical University, 2013. -





 下载:
下载: