Typing and antimicrobial resistance analysis of diarrheogenic Escherichia coli in Anhui Province from 2015 to 2019
-
摘要:
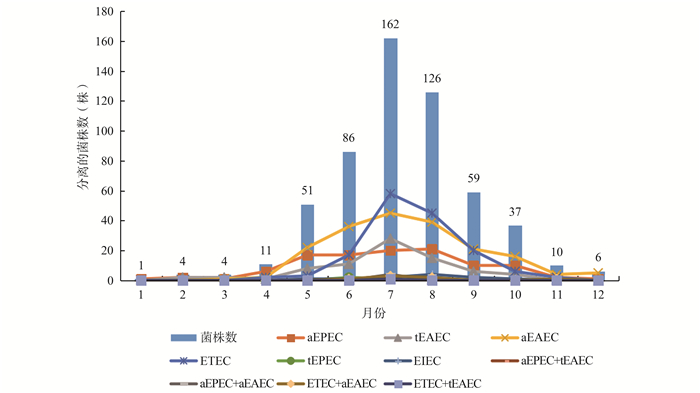
目的 了解安徽省致泻性大肠埃希菌(DEC)的菌群流行特点及耐药趋势,为安徽省DEC腹泻病的诊断和治疗提供科学依据。 方法 采集安徽省2015―2019年腹泻患者粪便样本,采用多重实时荧光定量PCR对细菌进行鉴定与分型,采用微量肉汤稀释法对细菌进行药敏试验。 结果 从6 120份粪便中分离出DEC 557株,主要病原型为:非典型肠聚集性大肠埃希菌(aEAEC)191(34.29%)株,产肠毒素性大肠埃希菌(ETEC)153(27.47%)株,非典型肠致病性大肠埃希菌(aEPEC)108(19.39%)株,典型肠聚集性大肠埃希菌(tEAEC)77(13.82%)株,肠侵袭性大肠埃希菌(EIEC)11(1.97%)株,典型肠致病性大肠埃希菌(tEPEC)3(0.54%)株。药敏检测多重耐药255(45.78%)株;同种病理类型不同年份耐药性存在差异:aEAEC:氨苄西林/舒巴坦(AMS),萘啶酸(NAL),头孢西林(CFZ);tEAEC:AMS,CFZ,阿奇霉素(AZM);EPEC(aEPEC,tEPEC):氨苄西林(AMP),AMS,CFZ;ETEC:NAL,AZM,环丙沙星(CIP)。不同病理类型耐药性存在差异的抗生素有:AMP,AMS,四环素(TET),NAL,红霉素(ERY),氯霉素(CHL),头孢噻肟(CTX),CFZ,庆大霉素(GEN),甲氧苄啶/磺胺甲恶唑(SXT),AZM和CIP。2015―2019年,tEAEC对CFZ,EPEC对AMP,AMS和CFZ,ETEC对NAL和CIP,耐药性呈增强趋势。 结论 本地区DEC流行的主要型别是:aEAEC、ETEC、aEPEC和tEAEC。DEC的耐药情况较严重,常用抗生素AMP、AMS、NAL、CFZ和CIP在不同年份和不同病理类型间,耐药性差异明显,耐药性分析结果为临床合理使用抗生素,遏制抗菌药物耐药性增加提供参考。 Abstract:Objective To understand the epidemic characteristics and drug resistance trend of diarrheogenic Escherichia coli (DEC) in Anhui area, so as to provide an important basis for prevention and treatment of DEC diarrhea in Anhui Province. Methods Fecal samples of diarrhea patients were collected and inoculated with McConkey culture medium in Anhui from 2015 to 2019. Suspicious colonies were identified and typed by multiple fluorescence quantitative PCR, and drug sensitivity test was carried out by microbroth dilution method. Results 557 strains were isolated from 6 120 stool samples. The main pathotypes were 191(34.29%) a typical enteroaggregative Escherichia coli (aEAEC), 153(27.47%) enterotoxigenic Escherichia coli (ETEC), 108(19.39%) a typical enteropathogenic Escherichia coli (aEPEC), 77(13.82%) typical enteroaggregative Escherichia coli (tEAEC), 11(1.97%) enteroinvasive Escherichia coli (EIEC) and 3(0.54%) typical enteropathogenic Escherichia coli (tEPEC). Multidrug resistant bacteria accounted for 45.78%. The statistically significant resistance difference of the same pathotype in different years were as follows:a typical EAEC:ampicillin/sulbactam (AMS), nalidixic acid (NAL), cefoxicillin (CFZ); typical EAEC:AMS, CFZ, azithromycin (AZM); EPEC:ampicillin (AMP), AMS, CFZ; ETEC:NAL, AZM, ciprofloxacin (CIP). The antibiotics with statistically significant differences in drug resistance among different pathotypes were AMP, AMS, tetracycline(TET), NAL, erythromycin (ERY), chloramphenicol (CHL), cefotaxime (CTX), CFZ, gentamicin (GEN), trimethoprim/sulfamethoxazole (SXT), AZM and CIP. The resistance of tEAEC to CFZ, EPEC to AMP, AMS and CFZ, ETEC to NAL and CIP showed an increasing trend from 2015 to 2019. Conclusions The mainly epidemic pathotypes in Anhui area were aEAEC, ETEC, aEPEC and tEAEC. The resistances of antibiotics (AMP, AMS, NAL, CFZ and CIP) were significantly different among different years and pathotypes. The results of resistance analysis can provide reference for rational use of antibiotics and prevention of the increase of antimicrobial resistance. -
Key words:
- Diarrheogenic Escherichia coli /
- Pathotypes /
- Resistance
-
表 1 2015―2019年安徽省557株致泻性大肠埃希氏菌的药敏检测结果
Table 1. Drug sensitivity results of 557 strains of diarrhea Escherichia coli in Anhui Province from 2015 to 2019
抗生素名称 耐药 中介 敏感 菌株数 百分率(%) 菌株数 百分率(%) 菌株数 百分率(%) AMP 399 71.63 6 1.08 152 27.29 CAZ 44 7.90 27 4.84 486 87.26 AMS 129 23.16 163 29.26 265 47.58 IPM 7 1.26 3 0.54 547 98.20 TET 303 54.40 5 0.90 249 44.70 NAL 318 57.09 - - 239 42.91 ERY 538 96.59 14 2.51 5 0.90 CFX 43 7.72 23 4.13 491 88.15 CHL 98 17.59 25 4.49 434 77.92 CTX 188 33.75 12 2.15 357 64.10 CFZ 230 41.29 110 19.75 217 38.96 GEN 143 25.67 13 2.33 401 72.00 SXT 270 48.47 - - 287 51.53 AZM 149 26.75 - - 408 73.25 CIP 79 14.18 12 2.16 466 83.66 注:AMP:氨苄西林;CAZ:头孢他啶;AMS:氨苄西林/舒巴坦;IPM:亚胺培南;TET:四环素;NAL:萘啶酸;ERY:红霉素;CFX:头孢西丁;CHL:氯霉素;CTX:头孢噻肟;CFZ:头孢唑啉;GEN:庆大霉素;SXT:甲氧苄啶/磺胺甲恶唑;AZM:阿奇霉素;CIP:环丙沙星。 表 2 安徽省同种病理类型DEC耐药性在2015―2019年间存在差异的结果[n(%)]
Table 2. Resistance difference of the same pathotype in Anhui Province from 2015 to 2019 [n(%)]
药敏
结果2015年 2016年 2017年 2018年 2019年 χ2值 P值 aEAEC AMS 24.626 0.002 R 5(13.16) 23(47.92) 10(31.25) 9(21.95) 11(34.38) I 8(21.05) 10(20.83) 8(25.00) 17(41.46) 13(40.62) S 25(65.79) 15(31.25) 14(43.75) 15(36.59) 8(25.00) NAL 10.074 0.039 R 24(63.16) 26(54.17) 27(84.38) 27(65.85) 25(78.13) S 14(36.84) 22(45.83) 5(15.62) 14(34.15) 7(21.87) CFZ 17.501 0.025 R 18(47.37) 24(50.00) 19(59.38) 17(41.46) 21(65.63) I 2(5.26) 13(27.08) 2(6.25) 9(21.95) 4(12.50) S 18(47.37) 11(22.92) 11(34.37) 15(36.59) 7(21.87) tEAEC AMS 17.049 0.030 R 0(0.00) 8(50.00) 3(20.00) 8(42.11) 6(31.58) I 1(12.5) 4(25.00) 7(46.67) 5(26.32) 9(47.37) S 7(87.50) 4(25.00) 5(33.33) 6(31.57) 4(21.05) CFZ 22.150 0.005 R 3(37.50) 2(12.50) 5(33.33) 12(63.16) 11(57.89) I 0(0.00) 9(56.25) 4(26.67) 1(5.26) 5(26.32) S 5(62.50) 5(31.25) 6(40.00) 6(31.58) 3(15.79) AZM 13.940 0.007 R 4(50.00) 5(31.25) 1(6.67) 11(57.89) 3(15.79) S 4(50.00) 11(68.75) 14(93.33) 8(42.11) 16(84.21) EPEC AMP 13.209 0.010 R 15(53.57) 9(33.33) 9(64.29) 13(81.25) 19(73.08) I 0(0.00) 0(0.00) 0(0.00) 0(0.00) 0(0.00) S 13(46.43) 18(66.67) 5(35.71) 3(18.75) 7(26.92) AMS 23.583 0.003 R 1(3.57) 6(22.22) 1(7.14) 6(37.50) 6(23.08) I 3(10.71) 3(11.11) 7(50.00) 5(31.25) 7(26.92) S 24(85.72) 18(66.67) 6(42.86) 5(31.25) 13(50.00) CFZ 32.965 <0.001 R 6(21.43) 5(18.52) 6(42.86) 9(56.25) 4(15.38) I 0(0.00) 5(18.52) 0(0.00) 4(25.00) 11(42.31) S 22(78.57) 17(62.96) 8(57.14) 3(18.7) 11(42.31) ETEC NAL 17.268 0.002 R 14(42.42) 14(42.42) 11(57.89) 46(75.41) 21(75.00) S 19(57.58) 19(57.58) 8(42.11) 15(24.59) 7(25.00) AZM 23.808 <0.001 R 3(9.09) 3(9.09) 4(21.05) 24(39.34) 1(3.57) S 30(90.91) 30(90.91) 15(78.95) 37(60.66) 27(96.43) CIP 23.364 0.003 R 0(0.00) 0(0.00) 3(15.79) 0(0.00) 4(14.29) I 0(0.00) 0(0.00) 0(0.00) 2(3.28) 0(0.00) S 33(100) 33(100) 16(84.21) 59(96.72) 24(85.71) 注:R:耐药;I:中介;S:敏感;aEAEC:非典型肠聚集性大肠埃希菌;tEAEC:典型肠聚集性大肠埃希菌;EPEC:肠致病性大肠埃希菌;ETEC:产肠毒素性大肠埃希菌;AMS:氨苄西林/舒巴坦;NAL:萘啶酸;CFZ:头孢唑啉;AZM:阿奇霉素;AMP:氨苄西林;CIP:环丙沙星 表 3 2015―2019年安徽省不同病理类型DEC耐药性存在差异的结果[n(%)]
Table 3. Resistance difference of different pathotypes in Anhui Province from 2015 to 2019 [n(%)]
药敏结果 aEAEC tEAEC EPEC (aEPEC, tEPEC) ETEC EIEC χ2值 P值 AMP 32.115 <0.001 R 149(78.01) 66(85.71) 65(58.56) 100(65.36) 11(72.73) I 1(0.52) 0(0.00) 0(0.00) 5(3.27) 0(0.00) S 41(21.47) 11(14.29) 46(41.44) 48(31.37) 3(27.27) AMS 35.558 <0.001 R 58(30.37) 25(32.47) 20(18.02) 16(10.46) 3(27.27) I 56(29.32) 26(33.77) 25(22.52) 52(33.99) 1(9.09) S 77(40.31) 26(33.76) 66(59.46) 85(55.56) 7(63.64) TET 39.860 <0.001 R 127(66.49) 42(54.55) 65(58.56) 52(33.99) 7(63.64) I 0(0.00) 1(1.30) 1(0.90) 3(1.96) 0(0.00) S 64(33.51) 34(44.15) 45(40.54) 98(64.05) 4(36.36) NAL 45.207 <0.001 R 129(67.54) 34(44.16) 36(32.43) 100(65.36) 6(54.55) S 62(32.46) 43(55.84) 75(67.57) 53(34.64) 5(45.45) ERY 22.707 0.004 R 187(97.91) 75(97.40) 110(99.10) 144(94.12) 9(81.82) I 4(2.09) 2(2.60) 1(0.90) 5(3.27) 2(18.18) S 0(0.00) 0(0.00) 0(0.00) 4(2.61) 0(0.00) CHL 39.536 <0.001 R 52(27.23) 8(10.39) 21(18.92) 10(6.54) 3(27.27) I 5(2.62) 9(11.69) 3(2.70) 7(4.57) 1(9.09) S 134(70.15) 60(77.92) 87(78.38) 136(88.89) 7(63.64) CTX 27.725 0.001 R 85(44.50) 26(33.77) 22(19.82) 42(27.45) 7(63.64) I 4(2.10) 1(1.30) 4(3.60) 3(1.96) 0(0.00) S 102(53.40) 50(64.93) 85(76.58) 108(70.59) 4(36.36) CFZ 30.436 <0.001 R 99(51.83) 33(42.86) 30(27.03) 54(35.29) 7(63.64) I 30(15.7) 19(2.68) 20(18.02) 38(24.84) 0(0.00) S 62(32.46) 25(32.46) 61(54.95) 61(39.87) 4(36.36) GEN 51.336 <0.001 R 73(38.22) 26(33.77) 28(25.23) 9(5.88) 4(36.36) I 5(2.62) 1(1.30) 2(1.80) 4(2.61) 0(0.00) S 113(59.16) 50(64.94) 81(72.97) 140(91.50) 7(63.64) SXT 74.453 <0.001 R 126(65.97) 49(63.64) 45(40.54) 35(22.88) 7(63.64) S 65(34.03) 28(36.36) 66(59.46) 118(77.12) 4(36.36) AZM 12.771 0.012 R 64(33.51) 24(31.17) 20(18.02) 32(20.92) 4(36.36) S 127(66.49) 53(68.83) 91(81.98) 121(79.08) 7(63.64) CIP 58.970 <0.001 R 52(27.23) 4(5.19) 9(8.11) 7(4.57) 4(36.36) I 3(1.57) 5(6.49) 2(1.80) 2(1.31) 0(0.00) S 136(71.20) 68(88.31) 100(90.09) 144(94.12) 7(63.64) 注:R:耐药;I:中介;S:敏感;AMP:氨苄西林;CAZ:头孢他啶;AMS:氨苄西林/舒巴坦;IPM:亚胺培南;TET:四环素;NAL:萘啶酸;ERY:红霉素;CFX:头孢西丁;CHL:氯霉素;CTX:头孢噻肟;CFZ:头孢唑啉;GEN:庆大霉素;SXT:甲氧苄啶/磺胺甲恶唑;AZM:阿奇霉素;CIP:环丙沙星;aEAEC:非典型肠聚集性大肠埃希菌;tEAEC:典型肠聚集性大肠埃希菌;aEPEC:非典型肠致病性大肠埃希菌;tEPEC:典型肠致病性大肠埃希菌;ETEC:产肠毒素性大肠埃希菌;EIEC:肠侵袭性大肠埃希菌。 -
[1] 朱旭慧, 周俞, 侯红艳, 等.急性腹泻患儿致泻性大肠埃希菌流行病学研究和耐药性分析[J].中华检验医学杂志, 2019, 42(3):214-218. DOI:10.3760/cma.j.issn. 1009-9158.2019.03.013.Zhu XH, Zhou Y, Hou HY, et al. Molecular epidemiology and antimicrobial resistance of diarrheagic Escherichia coli among children with acute diarrhea[J]. Chin J Lab Med, 2019, 42(3):214-218. DOI:10.3760/cma.j.issn. 1009-9158.2019.03.013. [2] 石挺丽, 黄建华, 李秀芬, 等. 2014-2015年广州地区腹泻患儿和健康儿童致泻性大肠埃希菌流行特征及耐药分析[J].中华疾病控制杂志, 2016, 20(4):329-332. DOI: 10.16462/j.cnki.zhjbkz.2016.04.002.Shi TL, Huang JH, Li XF, et al. Epidemiological characterization and antimicrobial resistance of diarrhea Escherichia coli from acute diarrheal and healthy children in Guangzhou City, 2014-2015[J]. Chin J Dis Control Prev, 2016, 20(4):329-332. DOI: 10.16462/j.cnki.zhjbkz.2016.04.002. [3] Zheng S, Yu F, Chen X, et al. Enteropathogens in children less than 5 years of age with acute diarrhea:a 5-year surveillance study in the Southeast Coast of China[J]. BMC Infect Dis, 2016, 16(1):434. DOI: 10.1186/s12879-016-1760-3. [4] Vijay D, Dhaka P, Vergis J, et al. Characterization and biofilm forming ability of diarrhoeagenic enteroaggregative Escherichia coli isolates recovered from human infants and young animals[J]. Comp Immunol Microbiol Infect Dis, 2015, 38:21-31. DOI: 10.1016/j.cimid.2014.11.004. [5] Hazen TH, Daugherty SC, Shetty AC, et al. Transcriptional variation of diverse enteropathogenic Escherichia coli isolates under virulence-inducing conditions[J]. mSystems. 2017, 2(4):1-19. DOI: 10.1128/mSystems.00024-17. [6] Fleckenstein JM, Hardwidge PR, Munson GP, et al. Molecular mechanisms of enterotoxigenic Escherichia coli infection[J]. Microbes Infect, 2010, 12(2):89-98. DOI:10.1016/j.micinf. 2009.10.002 [7] van den Beld MJC, Reubsaet FAG. Differentiation between Shigella, enteroinvasive Escherichia coli (EIEC) and noninvasive Escherichia coli[J]. Eur J Clin Microbiol Infect Dis, 2012, 31(6):899-904. DOI: 10.1007/s10096-011-1395-7. [8] 李春, 俞俊岭.安徽地区腹泻患者感染肠致病大肠埃希氏菌的耐药特征[J].中国人兽共患病学报, 2019, 35(8):732-737. DOI: 10.3969/ji.ssn.1002-2695.2019.00.136.LI C, Yu JL. Resistance characteristics of enteropathogenic Escherichia coli isolated fromf eces of diarrhea patients in Anhui, China[J]. Chin J Zoono, 2019, 35(8):732-737. DOI: 10.3969/ji.ssn.1002-2695.2019.00.136. [9] Zhang SX, Zhou YM, Tian LG, et al. Antibiotic resistance and molecular characterization of diarrheagenic Escherichia coli and non-typhoidal Salmonella strains isolated from infections in southwest China[J]. Infect Dis Poverty, 2018, 7(1):53. DOI: 10.1186/s40249-018-0427-2. [10] Huang Z, Pan H, Zhang P, et al. Prevalence and antimicrobial resistance patterns of siarrheagenic Escherichia coli in Shanghai, China[J]. Pediatr Infect Dis J, 2016, 35(8):835-839. DOI: 10.1097/INF.0000000000001190. [11] Chen Y, Chen X, Zheng S, et al. Serotypes, genotypes and antimicrobial resistance patterns of human diarrhoeagenic Escherichia coli isolates circulating in southeastern China[J]. Clin Microbiol Infect, 2014, 20(1):52-58. DOI: 10.1111/1469-0691.12188. [12] Haghi F, Zeighami H, Hajiahmadi F, et al. Frequency and antimicrobial resistance of diarrhoeagenic Escherichia coli from young children in Iran[J]. J Med Microbiol, 2014, 63(Pt 3), 427-432. DOI: 10.1099/jmm.0.064600-0. [13] Natarajan M, Kumar D, Mandal J, et al. A study of virulence and antimicrobial resistance pattern in diarrhoeagenic Escherichia coli isolated from diarrhoeal stool specimens from children and adults in a tertiary hospital, Puducherry, India[J]. J Health Popul Nutr, 2018, 37(1):17. DOI: 10.1186/s41043-018-0147-z. -





 下载:
下载: