-
摘要:
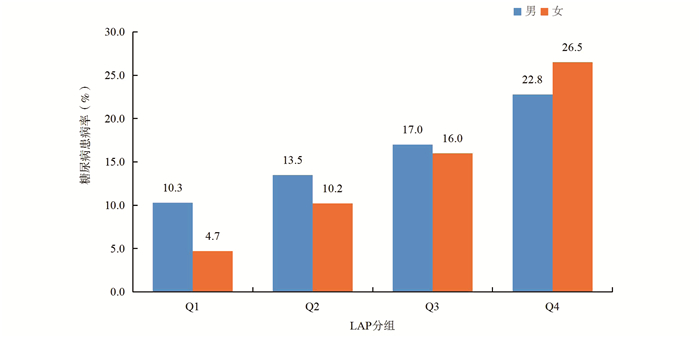
目的 探讨脂质蓄积指数(lipid accumulation product, LAP)与糖尿病患病风险的关系,并比较不同肥胖评价指标对糖尿病患病风险的预测价值。 方法 2016年6月―2017年12月,采取多阶段分层整群抽样的方法,选择上海市松江区4个社区20~74岁常住居民作为研究对象,对其进行问卷调查及体格、生化检查,并通过健康云平台获取体格检查前1年在区内医疗机构就诊记录。采用二分类Logistic回归分析模型探讨LAP与糖尿病的关系,通过计算受试者工作特征(receiver operating characteristic, ROC)曲线下面积(area under curve, AUC),比较各肥胖指标对糖尿病患病风险的预测价值。 结果 男女性FPG、糖化血红蛋白均随LAP的增加而增加(P < 0.05),LAP值最高的第四组(Q4组)男性和女性罹患糖尿病的风险分别是LAP值最低组(Q1组)的1.81倍(95% CI: 1.53~2.14)和2.87倍(95% CI: 2.43~3.40)。总人群LAP预测糖尿病患病风险的AUC大于BMI(P < 0.05)的AUC,且在女性中,LAP的AUC高于BMI和腰围(P < 0.05)的AUC,在男性和女性中的最佳截断值分别是23.30 cm·mmol/L和30.41 cm·mmol/L。 结论 LAP可用于糖尿病患病风险的预测,尤其在女性中预测价值更高。 Abstract:Objective To explore the relationship between lipid accumulation product (LAP) and the risk of diabetes among adults, and to compare the effectiveness of different obesity indicators in predicting diabetes. Methods A multi-stage stratified cluster sampling method was conducted among adults aged 20-74 in 4 communities in Songjiang District of Shanghai during June 2016 to December 2017. Questionnaire investigation, physical and biochemical examination were used to collect data. Logistic regression analysis models were used to evaluate the association LAP and diabetes, and receiver operating characteristics curve (ROC) was used to evaluate the predictive value of various obesity indicators in diabetes. Results The level of fasting blood glucose and HbA1c was increased with the increasing of LAP (P < 0.05). Compared to the first quintile of LAP level, risk of having diabetes in the fourth quintile were 1.81 times (95% CI: 1.53-2.14) for male and 2.87 times (95% CI: 2.43-3.40) for female respectively. The predictive value of LAP was higher than BMI (P < 0.05) both in male and female. It was also higher than waist circumference in female (P < 0.05). The cut-off point for LAP in predicting diabetes was 23.30 cm·mmol/L for male and 30.41 cm·mmol/L for female. Conclusion LAP could be used to predict the risk of diabetes, especially in women. -
Key words:
- Lipid accumulation product /
- Diabetes /
- Obesity
-
表 1 研究人群的基本特征[n(%)]
Table 1. Characteristics of survey population [n(%)]
变量 男性
(n=14 391)女性
(n=21 055)χ2/Z值 P值 年龄组(岁) 259.905 < 0.001 < 45 1 903(13.2) 3 147(15.0) 45~ < 55 3 304(23.0) 5 943(28.2) 55~ < 65 4 802(33.4) 6 992(33.2) ≥65 4 382(30.4) 4 973(23.6) 婚姻状况 127.949 < 0.001 在婚 13 637(94.8) 19 290(91.6) 非在婚a 754(5.2) 1 765(8.4) 受教育年限(年) 591.394 < 0.001 < 6 5 633(39.1) 10 930(51.9) 6~ < 10 7 878(54.7) 8 848(42.0) ≥10 880(6.2) 1 277(6.1) 吸烟 15 550.557 < 0.001 是 8 276(57.5) 63(0.3) 否 6 115(42.5) 20 992(99.7) 饮酒 7 176.681 < 0.001 是 4 607(32.0) 159(0.8) 否 9 784(68.0) 20 896(99.2) 锻炼 0.687 0.407 是 4 615(32.1) 6 663(31.7) 否 9 743(67.9) 14 340(68.3) BMI b
[kg/m2, M (P25~P75)]24.62
(22.57~26.74)23.92
(21.83~26.28)17.229 < 0.001 WC b
[cm, M (P25~P75)]85.00
(79.00~90.33)79.60
(73.00~86.00)49.530 < 0.001 WHR b
[%, M (P25~P75)]90.22
(86.60~93.55)86.75
(82.26~90.91)46.742 < 0.001 注:a非在婚包括未婚、离婚和丧偶;b采用Kruskal-Wallis H检验。 表 2 不同人群LAP分布情况[n(%)]
Table 2. LAP distribution in different populations [n(%)]
变量 男性 χ2/Z值 P值 女性 χ2/Z值 P值 Q1
(< 15.18)Q2
(15.18~ < 27.20)Q3
(27.20~ < 46.00)Q4
(≥46.00)Q1
(< 16.35)Q2
(16.35~ < 28.48)Q3
(28.48~ < 46.72)Q4
(≥46.72)年龄组(岁) 301.031 < 0.001 2 974.270 < 0.001 < 45 500(26.2) 414(21.8) 416(21.9) 573(30.1) 1 847(58.7) 673(21.4) 373(11.9) 254(8.0) 45~ < 55 645(19.5) 712(21.5) 844(25.5) 1 103(33.5) 1 623(27.3) 1 690(28.4) 1 374(23.1) 1 256(21.2) 55~ < 65 1 222(25.4) 1 251(26.1) 1 207(25.1) 1 122(23.4) 1 207(17.2) 1 780(25.5) 1 980(28.3) 2 025(29.0) ≥65 1 228(28.0) 1 216(27.7) 1 134(25.9) 804(18.4) 585(11.7) 1 119(22.5) 1 535(30.9) 1 734(34.9) 婚姻状况 48.384 < 0.001 1.757 0.624 在婚 3 332(24.4) 3 408(25.0) 3 464(25.4) 3 433(25.2) 4 811(24.9) 4 839(25.1) 4 828(25.0) 4 812(24.9) 非在婚 263(34.90) 185(24.5) 137(18.2) 169(22.4) 451(25.6) 423(24.0) 434(24.6) 457(25.8) 受教育年限(年) 128.759 < 0.001 1 702.999 < 0.001 < 6 1 567(27.8) 1 489(26.4) 1 402(24.9) 1 175(20.9) 1 743(15.9) 2 675(24.5) 3 158(28.9) 3 354(30.7) 6~ < 10 1 766(22.4) 1 890(24.0) 2 006(25.5) 2 216(28.1) 2 746(31.0) 2 330(26.3) 1 962(22.2) 1 810(20.5) ≥10 262(29.8) 214(24.3) 193(21.9) 211(24.0) 773(60.5) 257(20.1) 142(11.1) 105(8.3) 吸烟 12.537 0.006 6.645 0.084 是 2 104(25.4) 1 994(24.1) 2 045(24.7) 2 133(25.8) 16(25.4) 11(17.5) 12(19.0) 24(38.1) 否 1 491(24.4) 1 599(26.2) 1 556(25.4) 1 469(24.0) 5 246(25.0) 5 251(25.0) 5 250(25.0) 5 245(25.0) 饮酒 28.379 < 0.001 0.840 0.840 是 1 062(23.1) 1 133(24.6) 1 141(24.8) 1 271(27.6) 42(26.5) 43(27.0) 38(23.9) 36(22.6) 否 2 533(25.9) 2 460(25.1) 2 460(25.1) 2 331(23.9) 5 220(25.0) 5 219(25.0) 5 224(25.0) 5 233(25.0) 锻炼 24.627 < 0.001 8.589 0.035 是 1 034(22.4) 1 198(26.0) 1 180(25.5) 1 203(26.1) 1 702(25.5) 1 679(25.2) 1 699(25.5) 1 583(23.8) 否 2 554(26.2) 2 386(24.5) 2 412(24.8) 2 391(24.5) 3 552(24.8) 3 561(24.8) 3 553(24.8) 3 674(25.6) FPG
(mmol/L)4.64
(4.22~5.23)4.68
(4.24~5.33)4.75
(4.25~5.49)4.85
(4.32~5.71)155.81 < 0.001 4.61
(4.23~5.02)4.68
(4.23~5.26)4.79
(4.28~5.47)4.95
(4.36~5.82)570.947 < 0.001 糖化血红蛋白
(%)5.50
(5.20~5.80)5.60
(5.30~5.90)5.70
(5.40~6.00)5.80
(5.40~6.20)474.92 < 0.001 5.40
(5.10~5.70)5.60
(5.30~5.90)5.70
(5.40~6.00)5.90
(5.50~6.30)2 166.426 < 0.001 表 3 LAP与糖尿病患病关系的Logistic回归分析
Table 3. Logistic regression analysis of the relationship between LAP and diabetes
LAP
分组模型1 模型2 模型3 OR(95% CI)值 P值 OR(95% CI)值 P值 OR(95% CI)值 P值 男性 Q1 1.00 1.00 1.00 Q2 1.36(1.18~1.57) < 0.001 1.24(1.07~1.44) 0.005 1.08(0.93~1.27) 0.312 Q3 1.79(1.56~2.06) < 0.001 1.58(1.37~1.83) < 0.001 1.28(1.09~1.50) 0.003 Q4 2.57(2.25~2.93) < 0.001 2.45(2.13~2.83) < 0.001 1.81(1.53~2.14) < 0.001 女性 Q1 1.00 1.00 1.00 Q2 2.31(1.97~2.70) < 0.001 1.49(1.27~1.75) < 0.001 1.40(1.19~1.66) 0.001 Q3 3.86(3.33~4.48) < 0.001 2.08(1.78~2.43) < 0.001 1.80(1.52~2.12) < 0.001 Q4 7.31(6.34~8.42) < 0.001 3.63(3.13~4.22) < 0.001 2.87(2.43~3.40) < 0.001 总人群 Q1 1.00 1.00 1.00 Q2 1.74(1.57~1.93) < 0.001 1.33(1.20~1.49) < 0.001 1.20(1.07~1.34) 0.001 Q3 2.62(2.37~2.89) < 0.001 1.80(1.62~1.99) < 0.001 1.49(1.33~1.66) < 0.001 Q4 4.44(4.04~4.89) < 0.001 3.02(2.73~3.34) < 0.001 2.28(2.03~2.55) < 0.001 表 4 不同肥胖指标与糖尿病患病风险关系的ROC曲线分析
Table 4. ROC curve analysis of the relationship between different obesity indexes and the risk of diabetes
变量 AUC(95% CI) Z值 P值 总人群 LAP 0.645(0.640~0.651) BMI 0.631(0.626~0.637) 3.495 < 0.001 WC 0.639(0.633~0.644) 1.868 0.062 WHR 0.639(0.633~0.644) 1.553 0.120 男性 LAP 0.600(0.591~0.609) BMI 0.606(0.598~0.615) 1.051 0.293 WC 0.599(0.590~0.607) 0.322 0.748 WHR 0.598(0.589~0.607) 0.340 0.734 女性 LAP 0.682(0.675~0.689) BMI 0.648(0.641~0.655) 6.533 < 0.001 WC 0.668(0.661~0.675) 3.115 0.002 WHR 0.672(0.665~0.679) 1.933 0.053 注:Z值、P值为相应变量的AUC与由LAP获得的AUC比较的结果。 -
[1] Sung KC, Jeong WS, Wild SH, et al. Combined influence of insulin resistance, overweight/obesity, and fatty liver as risk factors for type 2 diabetes[J]. Diabetes Care, 2012, 35(4): 717-722. DOI: 10.2337/dc11-1853. [2] Chan JM, Rimm EB, Colditz GA, et al. Obesity, fat distribution, and weight gain as risk factors for clinical diabetes in men[J]. Diabetes Care, 1994, 17(9): 961-969. DOI: 10.2337/diacare.17.9.961. [3] Després JP. Intra-abdominal obesity: an untreated risk factor for type 2 diabetes and cardiovascular disease[J]. J Endocrinol Invest, 2006, 29(3 Suppl): 77-82. [4] 周伟, 丁聪聪, 祝玲娟, 等. 江西省居民不同肥胖指标对脑卒中风险的预测效果[J]. 中华疾病控制杂志, 2020, 24(9): 1021-1026. DOI: 10.16462/j.cnki.zhjbkz.2020.09.006.Zhou W, Ding CC, Zhu LJ, et al. Value of obesity indicators on risk prediction for stroke in Jiangxi Province[J]. Chin J Dis Control Prev, 2020, 24(9): 1021-1026. DOI: 10.16462/j.cnki.zhjbkz.2020.09.006. [5] 苏健, 吕淑荣, 杨婕, 等. 江苏省成人脂质蓄积指数与高血压和糖尿病患病风险关系的研究[J]. 中华疾病控制杂志, 2018, 22(3): 217-221, 271. DOI: 10.16462/j.cnki.zhjbkz.2018.03.002.Su J, Lyu SR, Yang J, et al. Relationship between lipid accumulation product and the risk of hypertension and diabetes in adults of Jiangsu Province[J]. Chin J Dis Control Prev, 2018, 22(3): 217-221, 271. DOI: 10.16462/j.cnki.zhjbkz.2018.03.002. [6] Kahn HS. The "lipid accumulation product" performs better than the body mass index for recognizing cardiovascular risk: a population-based comparison[J]. BMC Cardiovasc Disord, 2005, 5: 26. DOI: 10.1186/1471-2261-5-26. [7] Kahn HS. The lipid accumulation product is better than BMI for identifying diabetes: a population-based comparison[J]. Diabetes Care, 2006, 29(1): 151-153. DOI: 10.2337/diacare.29.1.151. [8] Bozorgmanesh M, Hadaegh F, Azizi F. Diabetes prediction, lipid accumulation product, and adiposity measures; 6-year follow-up: Tehran lipid and glucose study[J]. Lipids Health Dis, 2010, 9: 45. DOI: 10.1186/1476-511X-9-45. [9] Xu M, Huang M, Qiang D, et al. Hypertriglyceridemic waist phenotype and lipid accumulation product: two comprehensive obese indicators of waist circumference and triglyceride to predict type 2 diabetes mellitus in Chinese population[J]. J Diabetes Res, 2020, 2020: 9157430. DOI: 10.1155/2020/9157430. [10] Dong L, Lin M, Wang W, et al. Lipid accumulation product (LAP) was independently associatedwith obstructive sleep apnea in patients with type 2 diabetes mellitus[J]. BMC Endocr Disord, 2020, 20(1): 179. DOI: 10.1186/s12902-020-00661-x. [11] Zhao Q, Chen B, Wang R, et al. Cohort profile: protocol and baseline survey for the Shanghai Suburban Adult Cohort and Biobank (SSACB) study[J]. BMJ Open, 2020, 10(7): e35430. DOI: 10.1136/bmjopen-2019-035430. [12] Wakabayashi I, Daimon T. A strong association between lipid accumulation product and diabetes mellitus in japanese women and men[J]. J Atheroscler Thromb, 2014, 21(3): 282-288. DOI: 10.5551/jat.20628. [13] Tian T, Pei H, Chen Z, et al. Comparison of lipid accumulation product and body mass index as indicators of diabetes diagnosis among 215, 651 Chinese adults[J]. PeerJ, 2020, 8: e8483. DOI: 10.7717/peerj.8483. [14] 申元媛, 陈纪春, 李刚, 等. 北京市常住居民脂质蓄积指数与高血压、糖尿病的关系[J]. 中华预防医学杂志, 2017, 51(5): 415-420. DOI: 10.3760/cma.j.issn.0253-9624.2017.05.009.Shen YY, Chen JC, Li G, et al. Relationship of lipid accumulation product with hypertension and diabetes among Beijing residents study[J]. Chin J Prev Med, 2017, 51(5): 415-420. DOI: 10.3760/cma.j.issn.0253-9624.2017.05.009. [15] Blüher M. Obesity: global epidemiology and pathogenesis[J]. Nat Rev Endocrinol, 2019, 15(5): 288-298. DOI: 10.1038/s41574-019-0176-8. [16] 潘磊磊, 卢春明, 吴明, 等. 辽宁省35~75岁居民糖尿病患病率及影响因素[J]. 中华疾病控制杂志, 2020, 24(6): 670-675. DOI: 10.16462/j.cnki.zhjbkz.2020.06.010.Pan LL, Lu CM, Wu M, et al. Analysis on the diabetes prevalence and its influencing factors in population aged 35-75 years in Liaoning Province[J]. Chin J Dis Control Prev, 2020, 24(6): 670-675. DOI: 10.16462/j.cnki.zhjbkz.2020.06.010. [17] González-Muniesa P, Mártinez-González MA, Hu FB, et al. Obesity[J]. Nat Rev Dis Primers, 2017, 3: 17034. DOI: 10.1038/nrdp.2017.34. [18] 郭超, 尚文斌. 2型糖尿病患者内脏型肥胖与胰岛素抵抗的相关性研究进展[J]. 现代中西医结合杂志, 2015, 24(15): 1702-1704. DOI: 10.3969/j.issn.1008-8849.2015.15.041.Guo C, Shang WB. Research progress on correlation between visceral obesity and insulin resistance in type 2 diabetes mellitus[J]. Chin J Integr Tradit West Med, 2015, 24(15): 1702-1704. DOI: 10.3969/j.issn.1008-8849.2015.15.041. [19] 孙亮亮, 谢虹, 张艳芳, 等. 蚌埠市某地区成人脂质蓄积指数与糖尿病患病风险关系的研究[J]. 中华全科医学, 2019, 17(7): 1204-1208. DOI: 10.16766/j.cnki.issn.1674-4152.000902.Sun LL, Xie H, Zhang YF, et al. Relationship between lipid accumulation product and the risk of diabetes in adults of a region of Bengbu[J]. Chin J Gen Pract, 2019, 17(7): 1204-1208. DOI: 10.16766/j.cnki.issn.1674-4152.000902. [20] 程雯, 马志强, 张妍, 等. 2型糖尿病患者体脂分布与胰岛素抵抗的关系[J]. 诊断学理论与实践, 2011, 10(5): 479-481. DOI: 10.16150/j.1671-2870.2011.05.017.Cheng W, Ma ZQ, Zhang Y, et al. Relationship between body fat distribution and insulin resistance in type 2 diabetes[J]. J Diagn Concepts Pract, 2011, 10(5): 479-481. DOI: 10.16150/j.1671-2870.2011.05.017. [21] 张锐芝, 巢健茜, 徐辉, 等. 老年人肥胖与主要慢性病的关系[J]. 中华疾病控制杂志, 2017, 21(3): 233-236. DOI: 10.16462/j.cnki.zhjbkz.2017.03.005.Zhang RZ, Chao JQ, Chen H, et al. The relationship between obesity and the major chronic diseases in the elderly[J]. Chin J Dis Control Prev, 2017, 21(3): 233-236. DOI: 10.16462/j.cnki.zhjbkz.2017.03.005. [22] 张列强, 刘涛, 张兵兵, 等. 血脂异常和腹型肥胖的交互作用对糖尿病患病的关系研究[J]. 中国健康教育, 2019, 35(3): 212-215. DOI: 10.16168/j.cnki.issn.1002-9982.2019.03.005.Zhang LQ, Liu T, Zhang BB, et al. The influence of interaction between dyslipidemia and abdominal obesity on the prevalence of diabetes[J]. Chin J Heal Educ, 2019, 35(3): 212-215. DOI: 10.16168/j.cnki.issn.1002-9982.2019.03.005. [23] Nusrianto R, Ayundini G, Kristanti M, et al. Visceral adiposity index and lipid accumulation product as a predictor of type 2 diabetes mellitus: the Bogor cohort study of non-communicable diseases risk factors[J]. Diabetes Res Clin Pract, 2019, 155: 107798. DOI: 10.1016/j.diabres.2019.107798. -





 下载:
下载: