The mediating effect of glycohemoglobin in oxidative balance score and cognitive function in older adults
-
摘要:
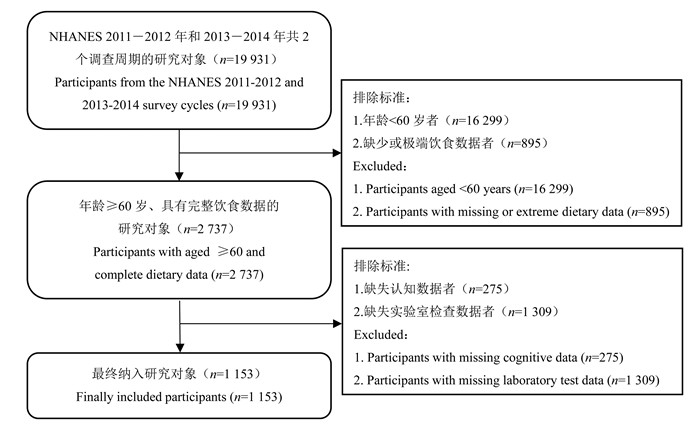
目的 探究糖化血红蛋白(glycosylated hemoglobin, HbA1c)在氧化平衡评分(oxidative balance score, OBS)与老年人认知功能关系中的中介效应,阐明抗氧化膳食和健康生活方式可能通过调控HbA1c水平影响认知功能的潜在机制,为基于糖代谢管理的认知健康干预策略提供理论依据。 方法 采用美国国家健康和营养调查数据进行分析,共纳入1 153例研究对象。运用logistic回归分析模型和限制性立方样条(restricted cubic spline, RCS)模型评估OBS和HbA1c水平与老年人认知功能之间的关联和剂量-反应关系,并采用逆概率加权的边际结构模型分析HbA1c水平在OBS与老年人认知功能之间的中介效应。 结果 高OBS为老年人认知功能的保护因素,高HbA1c水平为老年人认知功能的危险因素。RCS分析结果显示,OBS与老年人整体认知功能下降风险呈非线性剂量-反应关系(P非线性 < 0.001)。中介分析结果显示,OBS与老年人认知功能下降之间的关联由HbA1c部分介导。HbA1c水平在整体认知功能(OR=0.985, 95% CI: 0.975~0.996)、延迟回忆测试(OR=0.989, 95% CI: 0.981~0.999)和数字符号替代测试(OR=0.984, 95% CI: 0.974~0.996)中存在中介效应,其中介比例分别为17.6%、15.5%和23.9%。亚组分析结果显示,男性群体中HbA1c在OBS与老年人认知功能之间的关联性更强。 结论 OBS与老年人认知功能之间的关联由HbA1c部分介导,且存在性别差异,提示改善饮食结构可能成为预防认知衰退的重要策略。 Abstract:Objective This study investigated the mediating role of glycosylated hemoglobin (HbA1c) in the relationship between oxidative balance score (OBS) and cognitive function in older adults, aiming to elucidate the potential mechanisms through which antioxidant-rich diets and healthy lifestyles may influence cognitive performance via HbA1c regulation. The findings provide a theoretical foundation for developing cognitive health intervention strategies targeting glycemic control. Methods Data from the National Health and Nutrition Examination Survey were used to analyze this study, which included a total of 1 153 participants. The associations and dose-response relationships between OBS, HbA1c levels, and cognitive function were assessed using logistic regression models and restricted cubic spline (RCS) models, and the mediating effect of HbA1c level between OBS and cognitive function was analyzed using inverse probability-weighted marginal structural models. Results High OBS was a protective factor for cognitive function, whereas high HbA1c level was a risk factor for cognitive function. RCS showed a nonlinear dose-response relationship between OBS and the risk of overall cognitive function decline (Pnonlinear < 0.001). Mediation analysis show that the association between OBS and cognitive function decline was partially mediated by HbA1c. HbA1c levels were associated with a greater risk of cognitive function decline in overall cognitive function (OR=0.985, 95% CI: 0.975-0.996), DRT (OR=0.989, 95% CI: 0.981-0.999), and DSST (OR=0.984, 95% CI: 0.974-0.996) had a mediating proportions in 17.6%, 15.5%, and 23.9%, respectively. Subgroup analyses showed that the association of HbA1c between OBS and cognitive function was more significant in the male population. Conclusions The association between OBS and cognitive function was partially mediated by HbA1c and there were gender differences, it suggests that improving diet be an important strategy to prevent cognitive decline. -
Key words:
- Oxidative balance score /
- Cognitive function /
- Glycosylated hemoglobin /
- Elderly
-
图 3 不同性别老年人OBS与认知功能下降风险的剂量-反应关系
IRT:即时回忆测试;DRT:延迟回忆测试;AFT:动物流畅性测试;DSST:数字符号替代测试;OBS:氧化平衡评分。
Figure 3. Dose-response relationship between OBS and the risk of cognitive function decline among elderly individuals by gender
IRT: immediate recall test; DRT: delayed recall test; AFT: animal fluency test; DSST: digit symbol substitution test; OBS: oxidative balance score.
图 4 不同性别老年人HbA1c与认知功能下降风险的剂量-反应关系
IRT:即时回忆测试;DRT:延迟回忆测试;AFT:动物流畅性测试;DSST:数字符号替代测试;HbA1c:糖化血红蛋白。
Figure 4. Dose-response relationship between HbA1c and the risk of cognitive function decline among elderly individuals by gender
IRT: immediate recall test; DRT: delayed recall test; AFT: animal fluency test; DSST: digit symbol substitution test; HbA1c: glycosylated hemoglobin.
表 1 研究对象的一般人口学特征
Table 1. General demographic characteristics of the study participants
变量Variable 总数Total ①
(n=1 153)氧化平衡评分Oxidative balance score① χ2/F/H值value P值
valueQ1(n=421) Q2(n=351) Q3(n=381) 性别Gender 3.44 0.273 男Male 559(46.19) 202(42.56) 170(46.06) 187(49.15) 女Female 594(53.81) 219(57.44) 181(53.94) 194(50.85) 年龄组/岁Age group/years 19.06 0.041 60~ < 70 570(52.01) 192(44.61) 166(49.77) 212(59.64) 70~ < 80 326(27.02) 127(30.84) 108(29.07) 91(22.38) ≥80 257(20.97) 102(24.55) 77(21.16) 78(17.98) 种族Ethnicity 22.64 < 0.001 非西班牙裔白人Non-Hispanic White 614(82.05) 199(76.36) 197(82.18) 218(86.45) 非西班牙裔黑人Non-Hispanic Black 228(6.56) 112(10.97) 60(5.77) 56(3.73) 其他西班牙裔Other Hispanic 116(3.42) 47(4.80) 34(3.07) 35(2.61) 墨西哥裔美国人Mexican American 100(3.31) 33(3.58) 33(3.71) 34(2.76) 其他Others 95(4.66) 30(4.29) 27(5.27) 38(4.45) 受教育程度Level of education 66.65 < 0.001 高中以下Below high school level 278(15.67) 137(23.85) 77(13.82) 64(10.72) 高中High school 273(22.33) 115(26.40) 80(23.27) 78(18.37) 高中以上Above high school level 602(62.00) 169(49.75) 194(62.91) 239(70.91) 贫困比Poverty income ratio 43.09 < 0.001 <1.3 312(15.80) 132(20.91) 96(15.38) 84(12.10) 1.3~3.5 457(39.34) 185(47.73) 137(38.25) 135(33.61) >3.5 384(44.86) 104(31.36) 118(46.37) 162(54.29) 婚姻状况Marital status 25.05 0.077 离婚Divorced 128(10.79) 50(11.73) 42(12.30) 36(8.84) 与伴侣同住Living with partner 37(3.20) 15(4.75) 7(1.65) 15(3.24) 已婚Married 697(66.25) 245(59.08) 219(67.81) 233(70.64) 未婚Single 57(3.58) 18(2.59) 18(4.92) 21(3.28) 分居Separated 25(0.87) 12(1.18) 7(0.80) 6(0.67) 丧偶Widowed 209(15.31) 81(20.67) 58(12.52) 70(13.33) 吸烟状况Smoking status 22.89 0.007 现在吸烟Current smoker 121(9.12) 69(14.67) 33(8.82) 19(4.99) 过去吸烟Former smoker 457(42.22) 150(39.51) 142(40.89) 165(45.43) 从不吸烟Never smoker 575(48.66) 202(45.82) 176(50.29) 197(49.58) 体质量指数Body mass index/(kg·m-2) 32.38 0.006 过瘦Underweight (< 18.5) 15(1.38) 7(0.89) 2(1.25) 6(1.88) 正常Normal (18.5~ < 25.0) 298(27.57) 96(25.87) 74(19.28) 128(35.56) 超重Overweight (25.0~ < 30.0) 396(34.33) 146(32.13) 126(39.92) 124(31.59) 肥胖Obese (≥30.0) 444(36.72) 172(41.11) 149(39.55) 123(30.97) DII 462.61 < 0.001 抗炎饮食Anti-inflammatory diet 308(31.71) 2(0.90) 51(16.64) 255(68.03) 促炎饮食Proinflammatory diet 845(68.29) 419(99.10) 300(83.36) 126(31.97) 年龄组/岁Age group/years 69.1±6.6 70.1±6.5 69.1±6.6 68.4±6.5 6.51 0.004 收缩压Systolic blood pressure/mmHg 129.0±18.0 131.0±20.0 129.0±16.0 128.0±17.0 2.29 0.119 舒张压Diastolic blood pressure/mmHg 67.0±13.0 66.0±14.0 67.0±13.0 68.0±12.0 2.47 0.101 IRT 20(17, 23) 19(16, 22) 20(17, 23) 21(19, 24) 26.72 < 0.001 DRT 7(5, 8) 6(5, 8) 6(5, 8) 7(5, 8) 12.36 0.002 AFT 18(14, 22) 17(13, 20) 18(14, 21) 19(15, 23) 34.49 < 0.001 DSST 53(42, 64) 48(35, 59) 54(43, 64) 55(44, 67) 58.65 < 0.001 AIP 0.29±0.30 0.30±0.29 0.32±0.30 0.24±0.30 6.45 0.005 HbA1c/% 5.91±0.94 6.03±1.07 6.07±1.06 5.70±0.63 27.91 < 0.001 注:DII,膳食炎症指数;IRT,即时回忆测试;DRT,延迟回忆测试;AFT,动物流畅性测试;AIP,血浆致动脉硬化指数;HbA1c,糖化血红蛋白。
①以人数(占比/%)或x±s或M(P25, P75)表示。
Note: DII, dietary inflammatory index; IRT, immediate recall test; DRT, delayed recall test; AFT, animal fluency test; AIP, atherogenic index of plasma; HbA1c, glycosylated hemoglobin.
① Number of people (proportion/%) or x±s or M(P25, P75).表 2 OBS和HbA1c与认知功能的加权logistic回归
Table 2. Weighted logistic regression of OBS and HbA1c versus cognitive function
变量
Variable认知功能测试Cognitive function test IRT DRT AFT DSST 整体认知功能
Global cognitive functionOBS 0.94 (0.92~0.97)① 0.97 (0.94~1.00) 0.98 (0.95~1.01) 0.97 (0.95~1.00)③ 0.94 (0.91~0.97)① OBS分组Classification Q1 1.00 1.00 1.00 1.00 1.00 Q2 0.77 (0.51~1.18) 1.20 (0.75~1.92) 0.96 (0.59~1.55) 0.72 (0.42~1.24) 0.61 (0.36~1.01) Q3 0.49 (0.31~0.77)② 0.74 (0.44~1.24) 0.81 (0.51~1.30) 0.73 (0.50~1.05) 0.45 (0.27~0.76)② HbA1c 1.19 (0.98~1.46) 1.29 (1.07~1.54)② 1.18 (0.99~1.41) 1.28 (1.03~1.59)③ 1.32 (1.05~1.67)③ HbA1c分组Classification Q1 1.00 1.00 1.00 1.00 1.00 Q2 0.92 (0.62~1.37) 1.10 (0.78~1.57) 1.05 (0.71~1.56) 1.12 (0.66~1.90) 0.98 (0.63~1.53) Q3 1.17 (0.65~2.09) 1.55 (0.90~2.68) 1.52 (1.01~2.29)③ 1.39 (0.68~2.86) 1.50 (0.70~3.22) 注:OBS,氧化平衡评分;HbA1c,糖化血红蛋白;IRT,即时回忆测试;DRT,延迟回忆测试;AFT,动物流畅性测试;DSST,数字符号替代测试; 模型调整了年龄、性别、种族、受教育程度、婚姻状况、贫困比、体质量指数、吸烟状况。
① P < 0.001;② P < 0.01;③ P < 0.05。
Note: OBS, oxidative balance score; HbA1c, glycosylated hemoglobin; IRT, immediate recall test; DRT, delayed recall test; AFT, animal fluency test; DSST, digit symbol substitution test; The model was adjusted for age, gender, ethnicity, educational level, marital status, pverty income ratio, body mass index, and smoking status.
① P < 0.001; ② P < 0.01; ③ P < 0.05.表 3 HbA1c在OBS与认知障碍之间的中介效应
Table 3. The mediating effect of HbA1c on the relationship between OBS and cognitive impairment
分组
Classification结局变量
Outcome variable总效应
Total effect OR值value (95% CI)直接效应
Direct effect OR值value (95% CI)间接效应
Indirect effect OR值value (95% CI)中介比例
Mediation proportion合计Total 整体认知功能Overall cognitive function 0.915 (0.878~0.995)① 0.929 (0.891~0.969)① 0.985 (0.975~0.996)③ 17.6% IRT 0.945 (0.900~0.995)② 0.956 (0.908~1.005) 0.989 (0.981~0.999)② 20.0% DRT 0.932 (0.882~0.983)③ 0.942 (0.893~0.993)② 0.989 (0.981~0.999)② 15.5% AFT 0.954 (0.906~1.004) 0.967 (0.919~1.017) 0.987 (0.978~0.996)③ 27.1% DSST 0.933 (0.891~0.976)③ 0.948 (0.906~0.991)② 0.984 (0.974~0.996)③ 23.9% 男Male 整体认知功能Overall cognitive function 0.874 (0.814~0.938)① 0.900 (0.840~0.963)③ 0.971 (0.954~0.995)③ 23.0% IRT 0.890 (0.820~0.965)③ 0.908 (0.840~0.983)② 0.979 (0.965~0.996)② 19.1% DRT 0.915 (0.841~0.996)② 0.930 (0.856~1.010) 0.984 (0.969~1.001) 18.8% AFT 0.892 (0.831~0.959)③ 0.911 (0.850~0.977)③ 0.979 (0.965~0.999)② 19.4% DSST 0.922 (0.851~0.996)② 0.948 (0.879~1.023) 0.970 (0.953~0.995)③ 38.5% 女Female 整体认知功能Overall cognitive function 0.957 (0.912~1.003) 0.958 (0.916~1.003) 0.998 (0.981~1.011) 4.7% IRT 1.003 (0.944~1.067) 1.005 (0.946~1.068) 0.999 (0.987~1.010) -33.3% DRT 0.950 (0.891~1.015) 0.952 (0.893~1.016) 0.998 (0.981~1.014) 4.0% AFT 0.984 (0.915~1.059) 0.986 (0.919~1.059) 0.998 (0.981~1.011) 12.5% DSST 0.941 (0.899~0.984)③ 0.943 (0.902~0.984)③ 0.999 (0.982~1.011) 1.6% 注:模型调整了年龄、性别、种族、受教育程度、婚姻状况、贫困比; HbA1c,糖化血红蛋白;OBS,氧化平衡评分;IRT,即时回忆测试;DRT,延迟回忆测试;AFT,动物流畅性测试;DSST,数字符号替代测试。
① P < 0.001;② P < 0.05;③ P < 0.01。
Note: The model was adjusted for age, gender, ethnicity, educational level, marital status, and poverty income ratio; HbA1c, glycosylated hemoglobin; OBS, oxidative balance score; IRT, immediate recall test; DRT, delayed recall test; AFT, animal fluency test; DSST, digit symbol substitution test.
① P < 0.001;② P < 0.05;③ P < 0.01. -
[1] Daviglus ML, Bell CC, Berrettini W, et al. National institutes of health state-of-the-science conference statement: preventing Alzheimer disease and cognitive decline[J]. Ann Intern Med, 2010, 153(3): 176-181. DOI: 10.7326/0003-4819-153-3-201008030-00260. [2] Kivipelto M, Mangialasche F, Snyder HM, et al. World-wide FINGERS network: a global approach to risk reduction and prevention of dementia[J]. Alzheimers Dement, 2020, 16(7): 1078-1094. DOI: 10.1002/alz.12123. [3] Sanz-Blasco R, Ruiz-Sánchez de León JM, ávila-Villanueva M, et al. Transition from mild cognitive impairment to normal cognition: determining the predictors of reversion with multi-state Markov models[J]. Alzheimers Dement, 2022, 18(6): 1177-1185. DOI: 10.1002/alz.12448. [4] Yan MH, Wang XL, Zhu XW. Mitochondrial defects and oxidative stress in Alzheimer disease and Parkinson disease[J]. Free Radic Biol Med, 2013, 62: 90-101. DOI: 10.1016/j.freeradbiomed.2012.11.014. [5] Lei X, Xu ZX, Chen WW. Association of oxidative balance score with sleep quality: NHANES 2007-2014[J]. J Affect Disord, 2023, 339: 435-442. DOI: 10.1016/j.jad.2023.07.040. [6] Sheng LT, Jiang YW, Feng L, et al. Dietary total antioxidant capacity and late-life cognitive impairment: the Singapore Chinese health study[J]. J Gerontol A Biol Sci Med Sci, 2022, 77(3): 561-569. DOI: 10.1093/gerona/glab100. [7] Song LL, Li HR, Fu XH, et al. Association of the oxidative balance score and cognitive function and the mediating role of oxidative stress: evidence from the national health and nutrition examination survey (NHANES) 2011-2014[J]. J Nutr, 2023, 153(7): 1974-1983. DOI: 10.1016/j.tjnut.2023.05.014. [8] Wang YL, Zou CC, Na H, et al. Effect of different glucose monitoring methods on bold glucose control: a systematic review and meta-analysis[J]. Comput Math Methods Med, 2022, 2022: 2851572. DOI: 10.1155/2022/2851572. [9] Kanthi A, Singh D, Manjunath NK, et al. Changes in electrical activities of the brain associated with cognitive functions in type 2 diabetes mellitus: a systematic review[J]. Clin EEG Neurosci, 2024, 55(1): 130-142. DOI: 10.1177/15500594221089106. [10] Maan HB, Meo SA, Rouq FA, et al. Impact of Glycated Hemoglobin (HbA1c) on cognitive functions in type 2 diabetic patients[J]. Eur Rev Med Pharmacol Sci, 2021, 25: 5978-5985. DOI: 10.26355/eurrev_202110_26875. [11] Hegde SV, Adhikari P, Kotian SM, et al. The ABC (HbA1c, blood pressure and LDL-cholesterol) of diabetes and oxidative stress: knowing the links[J]. Biomedicine, 2022, 42(5): 925-928. DOI: 10.51248/.v42i5.2006. [12] Zhang W, Peng SF, Chen L, et al. Association between the oxidative balance score and telomere length from the national health and nutrition examination survey 1999-2002[J]. Oxid Med Cell Longev, 2022, 2022: 1345071. DOI: 10.1155/2022/1345071. [13] Brody DJ, Kramarow EA, Taylor CA, et al. Cognitive performance in adults aged 60 and over: national health and nutrition examination survey, 2011-2014[J]. Natl Health Stat Report, 2023, 126: 1-23. [14] Jaeger J. Digit symbol substitution test: the case for sensitivity over specificity in neuropsychological testing[J]. J Clin Psychopharmacol, 2018, 38(5): 513-519. DOI: 10.1097/JCP.0000000000000941. [15] Fillenbaum GG, Mohs R. CERAD (consortium to establish a registry for Alzheimer's disease) neuropsychology assessment battery 35 years and counting[J]. J Alzheimers Dis, 2023, 93(1): 1-27. DOI: 10.3233/JAD-230026. [16] Association AD. Standards of medical care in diabetes: 2021 abridged for primary care providers[J]. Clin Diabetes, 2021, 39(1): 14-43. DOI: 10.2337/cd21-as01. [17] Wang X, sarker Sk, Cheng L, et al. Association of dietary inflammatory potential, dietary oxidative balance score and biological aging[J]. Clinical Nutrition, 2024, 43(1): 1-10. DOI: 10.1016/j.clnu.2023.11.007. [18] Golmohammadi M, Ayremlou P, Zarrin R. Higher oxidative balance score is associated with better glycemic control among Iranian adults with type-2 diabetes[J]. Int J Vitam Nutr Res, 2021, 91(1-2): 31-39. DOI: 10.1024/0300-9831/a000596. [19] Kwon YJ, Park HM, Lee JH. Inverse association between oxidative balance score and incident type 2 diabetes mellitus[J]. Nutrients, 2023, 15(11): 2497. DOI: 10.3390/nu15112497. [20] Kim JS, Chun BC, Lee K. Association between elevated glycosylated hemoglobin and cognitive impairment in older Korean adults 2009-2010 Ansan cohort of the Korean genome and epidemiology study[J]. Front Public Health, 2024, 12: 1417236. DOI: 10.3389/fpubh.2024.1417236. [21] Casagrande SS, Lee C, Stoeckel LE, et al. Cognitive function among older adults with diabetes and prediabetes, NHANES 2011-2014[J]. Diabetes Res Clin Pract, 2021, 178: 108939. DOI: 10.1016/j.diabres.2021.108939. -





 下载:
下载: