Association between serum NHHR, AIP and the risk of chronic kidney disease: a prospective cohort study
-
摘要:
目的 评估血清非高密度脂蛋白胆固醇与高密度脂蛋白胆固醇比值(non-high density lipoprotein cholesterol/high density lipoprotein cholesterol, NHHR)、血浆致动脉粥样硬化指数(atherogenic index of plasma, AIP)与慢性肾病(chronic kidney disease, CKD)发病风险的关系, 为CKD的防治提供依据。 方法 以金昌队列中25 377名未患CKD的参与者作为研究对象, 采用Cox比例风险回归模型、限制性立方样条分别评估NHHR和AIP对CKD的发病风险及剂量-反应关系, 并进行亚组分析。采用受试者工作特征曲线评估NHHR和AIP对CKD发病风险的预测能力。 结果 经过平均4.77年的随访调查后, 新发CKD患者有1 213例, 发病密度为10.03/1 000人年。调整混杂因素后, 相较于Q1组, Q4组人群中NHHR和AIP的CKD发病风险比分别为1.270(95% CI: 1.066~1.512)和1.294(95% CI: 1.081~1.548), 且均存在一定的剂量-反应关系(均P<0.05)。NHHR和AIP预测CKD的AUC值分别为0.750(95% CI: 0.736~0.764)和0.735(95% CI: 0.721~0.749)。亚组分析发现, 吸烟和糖尿病与NHHR、糖尿病和AIP间存在交互作用(均P<0.05)。 结论 NHHR和AIP是CKD发病的独立危险因素, 并对CKD发病风险有一定的预测能力。 -
关键词:
- 非高密度脂蛋白胆固醇 /
- 高密度脂蛋白胆固醇 /
- 血浆致动脉粥样硬化指数 /
- 血脂代谢 /
- 慢性肾病 /
- 前瞻性队列研究
Abstract:Objective To analyse serum non-high-density lipoprotein cholesterol to high-density lipoprotein cholesterol ratio (NHHR), plasma atherogenic index (AIP) and the risk of chronic kidney disease (CKD). Methods A total of 25 377 participants without CKD from the Jinchang Cohort matched at baseline and follow-up were enrolled for the study. Cox proportional risk regression model and restricted cubic spline method were used to estimate the relationship between NHHR and AIP on the risk and dose response of CKD, and subgroup analyses were performed. Receiver operating characteristic curve and area under the curve (AUC) were conducted to evaluate the predictive ability on the risk of CKD. Results After an average follow-up period of 4.77 years, 1 213 new cases of CKD were identified, and the incidence density is 10.03/1 000 person-years. After adjusting for confounders, the HRs of NHHR and AIP in the Q4 population were 1.270 (95% CI: 1.066-1.512) and 1.294 (95% CI: 1.081-1.548), respectively, compared with the Q1 group, and all had dose-response relationship (all P < 0.05). The AUCs of NHHR and AIP for the prediction of CKD were 0.750 (95% CI: 0.736-0.764) and 0.735 (95% CI: 0.721-0.749), respectively. Subgroup analysis revealed interactions between smoking and diabetes with NHHR, and diabetes with AIP (all P < 0.05). Conclusions NHHR and AIP are independent risk factors for the development of CKD and have some predictive power with regard to the risk of CKD. -
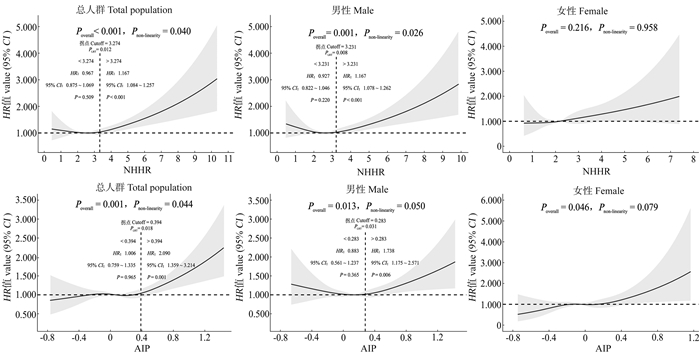
图 1 NHHR、AIP与CKD发病风险的剂量-反应关系
NHHR: 非高密度脂蛋白胆固醇与高密度脂蛋白胆固醇比值; AIP: 血浆致动脉粥样硬化指数; CKD: 慢性肾病; 模型调整了性别、年龄、职业、文化程度、个人月收入、吸烟、饮酒、体育锻炼、高盐饮食、高脂饮食、高糖饮食、体质量指数、高血压、糖尿病、高尿酸血症、基线估算的肾小球滤过率、谷丙转氨酶、谷草转氨酶和血红蛋白。
Figure 1. Dose-response relationship between NHHR, AIP and risk of CKD
NHHR: non-high density lipoprotein cholesterol/high density lipoprotein cholesterol; AIP: atherogenic index of plasma; CKD: chronic kidney disease; Models adjusted for gender, age, occupation, education, individual monthly incomes, smoking, drinking, physical exercise, high salt diet, high fat diet, high sugar diet, body mass index, hypertension, diabetes, hyperuricemia, baseline estimated-glomerular filtration rate, alanine aminotransferase, aspartate aminotransferase, and hemoglobin on the basis of model 2.
图 2 NHHR和AIP预测CKD发病风险的ROC曲线
NHHR: 非高密度脂蛋白胆固醇与高密度脂蛋白胆固醇比值; AIP: 血浆致动脉粥样硬化指数; CKD: 慢性肾病; AUC: 曲线下面积。
Figure 2. ROC curves of NHHR and AIP for predicting the risk of CKD
NHHR: non-high density lipoprotein cholesterol/high density lipoprotein cholesterol; AIP: atherogenic index of plasma; CKD: chronic kidney disease; AUC: area under the curve.
图 3 NHHR、AIP与CKD发病风险关联的亚组分析
NHHR: 非高密度脂蛋白胆固醇与高密度脂蛋白胆固醇比值; AIP: 血浆致动脉粥样硬化指数; CKD: 慢性肾病。
Figure 3. Subgroup analysis of the association between NHHR, AIP, and risk of CKD
NHHR: non-high density lipoprotein cholesterol/high density lipoprotein cholesterol; AIP: atherogenic index of plasma; CKD: chronic kidney disease.
表 1 研究对象的基线特征
Table 1. Baseline characteristics of the participants
变量Variable 非CKD组
Non-CKD group
(n=24 164)①CKD组
CKD group
(n=1 213)①Z/χ2
值valueP值
value性别Gender 101.82 0.001 男Male 14 462(59.85) 902(74.36) 女Female 9 702(40.15) 311(25.64) 年龄/岁Age/years 44.00(39.00, 55.00) 48.00(41.00, 65.00) -11.33 0.001 职业Occupation 11.05 0.011 工人Worker 19 468(80.57) 1 011(83.35) 干部Managerial staff 2 752(11.39) 106(8.74) 技术人员Technical staff 999(4.13) 41(3.38) 内勤人员Logistics staff 945(3.91) 55(4.53) 文化程度Education 80.98 < 0.001 初中及以下Junior middle school or below 9 546(39.50) 621(51.19) 高中或中专Senior middle school or equivalent 6 758(27.97) 327(26.96) 大专及以上College or above 7 860(32.53) 265(21.85) 个人月收入/元Individual monthly incomes/yuan 8.14 0.005 ≥2 000 12 613(52.20) 684(56.39) < 2 000 11 551(47.80) 529(43.61) 体质量指数Body mass index/(kg·m-2) 23.34(21.21, 25.61) 24.68(22.45, 26.97) -12.04 < 0.001 吸烟Smoking 103.45 < 0.001 从不Never 13 340(55.21) 521(42.95) 仍然Still 8 879(36.74) 513(42.29) 戒烟Quit 1 945(8.05) 179(14.76) 饮酒Drinking 87.09 < 0.001 从不Never 18 173(75.21) 789(65.04) 偶尔Occasionally 4 974(20.58) 318(26.22) 经常Regular 1 017(4.21) 106(8.74) 体育锻炼Physical exercise 8.93 0.012 从不Never 2 161(8.94) 139(11.46) 偶尔Occasionally 10 285(42.56) 498(41.05) 经常Regular 11 718(48.50) 576(47.49) 高盐饮食High salt diet 5 496(22.74) 281(23.17) 0.12 0.759 高脂饮食High fat diet 4 680(19.37) 246(20.28) 0.61 0.455 高糖饮食High sugar diet 4 877(20.18) 232(19.13) 0.80 0.390 高血压Hypertension 6 363(26.33) 612(50.45) 337.17 < 0.001 糖尿病Diabetes 1 567(6.48) 258(21.27) 378.27 < 0.001 高尿酸血症Hyperuricemia 2 738(11.33) 234(19.29) 70.78 < 0.001 血清尿酸Serum uric acid/(μmol·L-1) 316.00(263.00, 373.00) 345.00(294.00, 402.00) -11.66 < 0.001 血清肌酐Serum creatinine/(μmol·L-1) 68.50(59.00, 77.00) 72.00(62.00, 83.00) -9.48 < 0.001 谷丙转氨酶Alanine aminotransferase/(U·L-1) 27.00(19.00, 40.00) 30.00(21.00, 45.00) -6.61 < 0.001 谷草转氨酶Aspartate aminotransferase/(U·L-1) 31.00(26.00, 38.00) 33.00(27.00, 41.00) -5.94 < 0.001 收缩压Systolic blood pressure/mmHg 121.00(109.00, 134.00) 131.00(119.00, 146.00) -17.14 < 0.001 舒张压Diastolic blood pressure/mmHg 77.00(70.00, 86.00) 83.00(75.00, 93.00) -15.32 < 0.001 空腹血糖Fasting plasma glucose/(mmol·L-1) 5.10(4.70, 5.50) 5.40(4.90, 6.20) -15.22 < 0.001 碱性磷酸酶Alkaline phosphatase/(U·L-1) 65.00(54.00, 79.00) 68.00(56.00, 81.00) -4.55 < 0.001 血红蛋白Hemoglobin/(g·L-1) 151.00(139.00, 161.00) 158.00(151.00, 165.00) -18.16 < 0.001 基线e-GFR Baseline e-GFR/(mL·min-1·1.73m-2) 105.00(94.95, 112.55) 101.28(85.77, 111.34) -9.36 < 0.001 总胆固醇Total cholesterol/(mmol·L-1) 4.60(4.10, 5.20) 4.70(4.20, 5.40) -4.46 < 0.001 三酰甘油Triglyceride/(mmol·L-1) 1.50(1.10, 2.30) 1.80(1.30, 2.70) -9.49 < 0.001 HDL-C/(mmol·L-1) 1.33(1.13, 1.57) 1.27(1.07, 1.51) -6.45 < 0.001 LDL-C/(mmol·L-1) 3.02(2.56, 3.51) 3.12(2.62, 3.62) -3.68 < 0.001 NHHR 2.46(1.88, 3.14) 2.71(2.12, 3.49) -9.12 < 0.001 AIP 0.06(-0.14, 0.28) 0.15(-0.05, 0.37) -9.63 < 0.001 注: CKD, 慢性肾病; e-GFR, 估算的肾小球滤过率; HDL-C, 高密度脂蛋白胆固醇; LDL-C, 低密度脂蛋白胆固醇; NHHR, 非HDL-C与HDL-C比值; AIP, 血浆致动脉粥样硬化指数。
①以人数(占比/%)或M(P25, P75)表示。
Note: CKD, chronic kidney disease; e-GFR, estimated-glomerular filtration rate; HDL-C, high density lipoprotein cholesterol; LDL-C, low density lipoprotein cholesterol; NHHR, non-HDL-C/HDL-C; AIP, atherogenic index of plasma.
① Number of people (proportion/%) or M(P25, P75).表 2 NHHR、AIP对CKD发病风险的影响
Table 2. Influence of NHHR and AIP on the risk of CKD
变量
Variable模型1 Model 1 模型2 Model 2 模型3 Model 3 HR值value(95% CI) P值value HR值value(95% CI) P值value HR值value(95% CI) P值value NHHR① 1.170(1.116~1.227) < 0.001 1.123(1.065~1.183) < 0.001 1.083(1.026~1.144) 0.004 Q1 1.000 1.000 1.000 Q2 1.260(1.053~1.507) 0.012 1.103(0.921~1.321) 0.289 1.072(0.895~1.285) 0.450 Q3 1.506(1.267~1.790) < 0.001 1.215(1.019~1.449) 0.030 1.182(0.991~1.410) 0.064 Q4 1.922(1.629~2.267) < 0.001 1.456(1.227~1.727) < 0.001 1.270(1.066~1.512) 0.007 AIP① 1.215(1.149~1.285) < 0.001 1.149(1.082~1.219) < 0.001 1.087(1.022~1.157) 0.008 Q1 1.000 1.000 1.000 Q2 1.210(1.008~1.453) 0.041 1.199(0.998~1.439) 0.052 1.140(0.949~1.369) 0.163 Q3 1.319(1.103~1.577) 0.002 1.308(1.093~1.564) 0.003 1.155(0.964~1.385) 0.119 Q4 1.610(1.354~1.914) < 0.001 1.576(1.324~1.876) < 0.001 1.294(1.081~1.548) 0.005 注: NHHR, 非高密度脂蛋白胆固醇与高密度脂蛋白胆固醇比值; AIP, 血浆致动脉粥样硬化指数; CKD, 慢性肾病; 模型1调整了性别和年龄; 模型2在模型1的基础上进一步调整了职业、文化程度、个人月收入、吸烟、饮酒、体育锻炼、高盐饮食、高脂饮食、高糖饮食和体质量指数; 模型3在模型2的基础上进一步调整了高血压、糖尿病、高尿酸血症、基线估算的肾小球滤过率、谷丙转氨酶、谷草转氨酶和血红蛋白。
①代表指标作为连续型变量, 每增加1个标准差时CKD的HR(95% CI)值。
Note: NHHR, non-high density lipoprotein cholesterol/high density lipoprotein cholesterol; AIP, atherogenic index of plasma; CKD, chronic kidney disease; Model 1 adjusted for gender and age; Model 2 further adjusted for occupation, education, individual monthly incomes, smoking, drinking, physical exercise, high salt diet, high fat diet, high sugar diet, and body mass index on the basis of model 1; and model 3 further adjusted for hypertension, diabetes, hyperuricemia, baseline estimated-glomerular filtration rate, alanine aminotransferase, aspartate aminotransferase, and hemoglobin on the basis of model 2.
① Represents the HR (95% CI) values for CKD for each 1 standard deviation increase in the representative indicator as a continuous variable. -
[1] Lyu K, Liu YL, Zhang XF, et al. Prevalence of chronic kidney disease in a city of Northwestern China: a cross-sectional study[J]. Int Urol Nephrol, 2023, 55(8): 2035-2045. DOI: 10.1007/s11255-023-03515-2. [2] Ene-Iordache B, Perico N, Bikbov B, et al. Chronic kidney disease and cardiovascular risk in six regions of the world (ISN-KDDC): a cross-sectional study[J]. Lancet Glob Health, 2016, 4(5): e307-19. DOI: 10.1016/S2214-109X(16)00071-1. [3] Opazo-Ríos L, Mas S, Marín-Royo G, et al. Lipotoxicity and diabetic nephropathy: novel mechanistic insights and therapeutic opportunities[J]. Int J Mol Sci, 2020, 21(7): 2632. DOI: 10.3390/ijms21072632. [4] Nakano T, Tanaka S, Tsuruya K, et al. Relationship between serum lipid concentrations and impaired renal function in patients with chronic kidney disease: the fukuoka kidney disease registry study[J]. Clin Exp Nephrol, 2021, 25(4): 385-393. DOI: 10.1007/s10157-020-02000-9. [5] Weldegiorgis M, Woodward M. Elevated triglycerides and reduced high-density lipoprotein cholesterol are independently associated with the onset of advanced chronic kidney disease: a cohort study of 911 360 individuals from the United Kingdom[J]. BMC Nephrol, 2022, 23(1): 312. DOI: 10.1186/s12882-022-02932-2. [6] Zhang YB, Sheng LT, Wei W, et al. Association of blood lipid profile with incident chronic kidney disease: a Mendelian randomization study[J]. Atherosclerosis, 2020, 300: 19-25. DOI: 10.1016/j.atherosclerosis.2020.03.020. [7] Wang BX, Li LY, Tang Y, et al. Changes in non-high-density lipoprotein to high-density lipoprotein ratio (NHHR) and cardiovascular disease: insights from CHARLS[J]. Lipids Health Dis, 2025, 24(1): 112. DOI: 10.1186/s12944-025-02536-3. [8] Min QQ, Wu ZG, Yao JN, et al. Association between atherogenic index of plasma control level and incident cardiovascular disease in middle-aged and elderly Chinese individuals with abnormal glucose metabolism[J]. Cardiovasc Diabetol, 2024, 23(1): 54. DOI: 10.1186/s12933-024-02144-y. [9] Shi YM, Wen MH. Sex-specific differences in the effect of the atherogenic index of plasma on prediabetes and diabetes in the NHANES 2011-2018 population[J]. Cardiovasc Diabetol, 2023, 22(1): 19. DOI: 10.1186/s12933-023-01740-8. [10] Yu BY, Li M, Yu ZL, et al. The non-high-density lipoprotein cholesterol to high-density lipoprotein cholesterol ratio (NHHR) as a predictor of all-cause and cardiovascular mortality in US adults with diabetes or prediabetes: NHANES 1999-2018[J]. BMC Med, 2024, 22(1): 317. DOI: 10.1186/s12916-024-03536-3. [11] Giavarina D, Husain-Syed F, Ronco C. Clinical implications of the new equation to estimate glomerular filtration rate[J]. Nephron, 2021, 145(5): 508-512. DOI: 10.1159/000516638. [12] Ding LL, Zhu XH, Xiong ZF, et al. The association of age at diagnosis of hypertension with cognitive decline: the China health and retirement longitudinal study (CHARLS)[J]. J Gen Intern Med, 2023, 38(6): 1431-1438. DOI: 10.1007/s11606-022-07951-1. [13] 中华医学会糖尿病学分会. 中国2型糖尿病防治指南(2020年版)[J]. 国际内分泌代谢杂志, 2021, 41(5): 482-548. DOI: 10.3760/cma.j.cn121383-20210825-08063.Chinese Diabetes Society. Guideline for the prevention and treatment of type 2 diabetes mellitus in China (2020 edition)[J]. Int J Endocrinol Metab, 2021, 41(5): 482-548. DOI: 10.3760/cma.j.cn121383-20210825-08063. [14] 中华医学会内分泌学分会. 中国高尿酸血症与痛风诊疗指南(2019)[J]. 中华内分泌代谢杂志, 2020, 36(1): 1-13. DOI: 10.3760/cma.j.issn.1000-6699.2020.01.001.Society of Endocrinology, Chinese Medical Association. Guideline for the diagnosis and management of hyperuricemia and gout in China (2019)[J]. Chin J Endocrinol Metab, 2020, 36(1): 1-13. DOI: 10.3760/cma.j.issn.1000-6699.2020.01.001. [15] Hao JQ, Zhuang ZX, Hu SY, et al. The association between non-high-density lipoprotein cholesterol to high-density lipoprotein cholesterol ratio (NHHR) and low muscle mass in adults aged 20-59: a population-based study in the United States[J]. Lipids Health Dis, 2024, 23(1): 274. DOI: 10.1186/s12944-024-02243-5. [16] Wu J, Zhou Q, Wei ZX, et al. Atherogenic index of plasma and coronary artery disease in the adult population: a meta-analysis[J]. Front Cardiovasc Med, 2021, 8: 817441. DOI: 10.3389/fcvm.2021.817441. [17] Liu YL, Lyu K, Liu SD, et al. Predictive value of total cholesterol to high-density lipoprotein cholesterol ratio for chronic kidney disease among adult male and female in Northwest China[J]. Chronic Dis Transl Med, 2024, 10(3): 216-226. DOI: 10.1002/cdt3.122. [18] Sheng GT, Liu DY, Kuang MB, et al. Utility of non-high-density lipoprotein cholesterol to high-density lipoprotein cholesterol ratio in evaluating incident diabetes risk[J]. Diabetes Metab Syndr Obes, 2022, 15: 1677-1686. DOI: 10.2147/DMSO.S355980. [19] Lyu K, Liu SD, Liu YL, et al. The effect of blood lipid profiles on chronic kidney disease in a prospective cohort: based on a regression discontinuity design[J]. Biomed Environ Sci, 2024, 37(10): 1158-1172. DOI: 10.3967/bes2024.113. [20] Nguyen HH, Tran HH, Nguyen LT, et al. TG/HDL-C ratio is a risk factor associated with CKD: use in assessing the risk of progression of CKD[J]. Pathophysiology, 2022, 29(3): 374-382. DOI: 10.3390/pathophysiology29030029. [21] Li W, Du ZJ, Wei HL, et al. Total cholesterol to high-density lipoprotein cholesterol ratio is independently associated with CKD progression[J]. Int Urol Nephrol, 2022, 54(8): 2057-2063. DOI: 10.1007/s11255-021-03099-9. [22] Tsuruya K, Yoshida H, Nagata M, et al. Impact of the triglycerides to high-density lipoprotein cholesterol ratio on the incidence and progression of CKD: a longitudinal study in a large Japanese population[J]. Am J Kidney Dis, 2015, 66(6): 972-983. DOI: 10.1053/j.ajkd.2015.05.011. [23] Oh D, Lee S, Yang E, et al. Atherogenic indices and risk of chronic kidney disease in metabolic derangements: Gangnam Severance Medical Cohort[J]. Kidney Res Clin Pract, 2025, 44(1): 132-144. DOI: 10.23876/j.krcp.23.043. [24] Aggarwal DJ, Kathariya MG, Verma DPK. LDL-C, NON-HDL-C and APO-B for cardiovascular risk assessment: looking for the ideal marker[J]. Indian Heart J, 2021, 73(5): 544-548. DOI: 10.1016/j.ihj.2021.07.013. [25] Kraaijenhof JM, Hovingh GK, Stroes ESG, et al. The iterative lipid impact on inflammation in atherosclerosis[J]. Curr Opin Lipidol, 2021, 32(5): 286-292. DOI: 10.1097/MOL.0000000000000779. [26] Chabowski DS, Cohen KE, Abu-Hatoum O, et al. Crossing signals: bioactive lipids in the microvasculature[J]. Am J Physiol Heart Circ Physiol, 2020, 318(5): H1185-H1197. DOI: 10.1152/ajpheart.00706.2019. [27] Wang X, He B. Insight into endothelial cell-derived extracellular vesicles in cardiovascular disease: molecular mechanisms and clinical implications[J]. Pharmacol Res, 2024, 207: 107309. DOI: 10.1016/j.phrs.2024.107309. -





 下载:
下载: